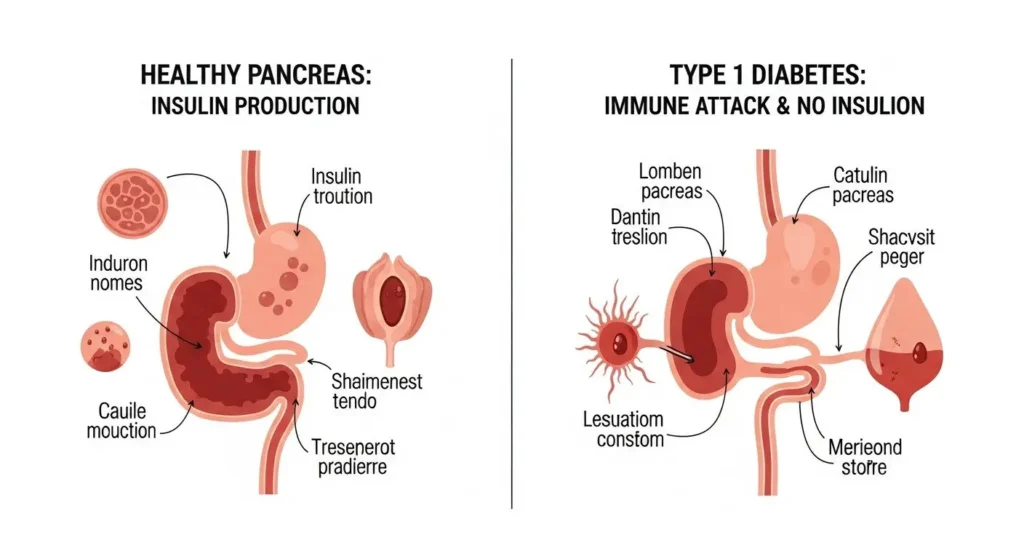
Type 1 diabetes (T1D) is a serious, lifelong condition that affects millions of people worldwide. Unlike its more commonly discussed cousin, type 2 diabetes, T1D isn't caused by lifestyle choices. It's an autoimmune disease, meaning the body's own immune system mistakenly attacks and destroys the cells in the pancreas that produce insulin. This leaves the body unable to make insulin, a vital hormone needed to turn sugar (glucose) from food into energy.
Living with Type 1 diabetes (T1D) means a daily balancing act of insulin, diet, and activity, but with the right knowledge and tools, individuals can lead full and active lives. Advancements in technology and understanding continue to make managing this condition more effective than ever before.
Key Takeaways
- Type 1 Diabetes is Autoimmune: T1D is an autoimmune disease where the body attacks its own insulin-producing cells, not caused by diet or lifestyle.
- Insulin is Essential: People with T1D must take insulin every day, either through injections or an insulin pump, as their body cannot produce it.
- Constant Management is Key: Managing T1D involves carefully balancing insulin doses, food intake (especially carbohydrates), and physical activity to keep blood sugar levels stable.
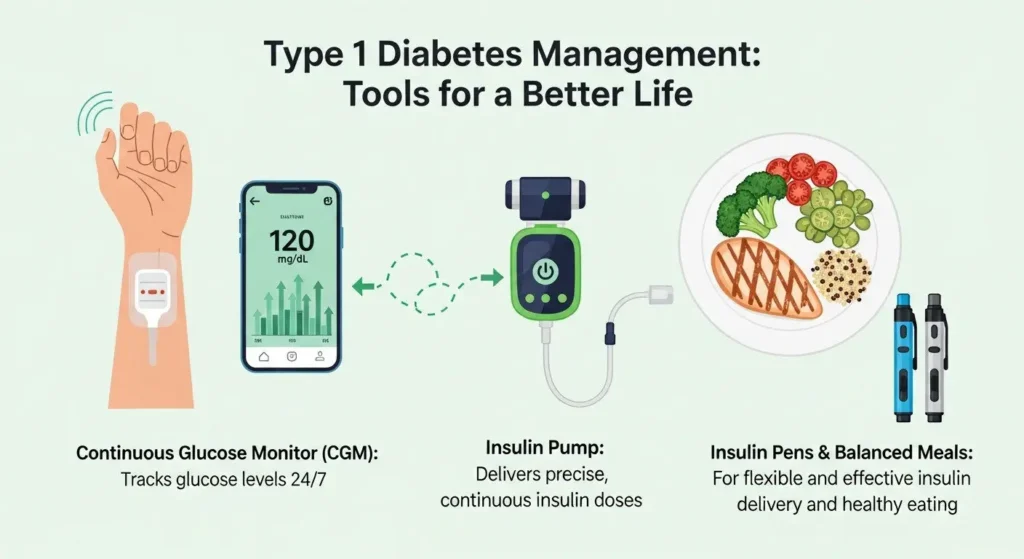
- Modern Tech Helps: Technologies like continuous glucose monitors (CGMs) and advanced insulin pumps have made managing T1D much easier and more precise.
- Support and Education Empower: Understanding T1D, debunking myths, and accessing support networks are crucial for living well with the condition.
What Exactly is Type 1 Diabetes?
Imagine your body as a car. To run, this car needs fuel (sugar from food) and a key to unlock the fuel tank so the fuel can get to the engine and be used. In your body, sugar (glucose) is the fuel, and insulin is the key. Insulin is a hormone made by special cells in your pancreas called beta cells. It helps glucose move from your bloodstream into your cells, where it's used for energy.
For someone with Type 1 Diabetes, their immune system, which is supposed to protect them from germs, gets confused. It sees these helpful beta cells in the pancreas as a threat and attacks them, eventually destroying most or all of them. This means the pancreas can no longer make insulin. Without insulin, glucose builds up in the bloodstream because it can't get into the cells. This high blood sugar can cause many serious health problems if not managed.
It's important to understand that T1D is an autoimmune disease. This means it's not something you get from eating too much sugar, being overweight, or not exercising enough. These factors are often linked to type 2 diabetes, which is a very different condition. You can learn more about the differences between these conditions by exploring Type 2 vs. Type 1 Diabetes.
Key Differences from Type 2 Diabetes
| Feature | Type 1 Diabetes | Type 2 Diabetes |
|---|---|---|
| Cause | Autoimmune destruction of insulin-producing cells | Insulin resistance (body doesn't use insulin well) or insufficient insulin production |
| Onset | Often sudden, typically in children/young adults (but can occur at any age) | Gradual, often in adults (but increasing in children) |
| Insulin Production | None or very little | Some insulin produced, but not enough or not used effectively |
| Treatment | Always requires insulin therapy | May be managed with diet, exercise, oral medications; sometimes insulin |
| Prevention | Currently no known way to prevent | Often preventable or delayable with lifestyle changes |
Who Gets Type 1 Diabetes?
Anyone can develop Type 1 Diabetes, regardless of age, ethnicity, or gender. While it's most commonly diagnosed in children, teenagers, and young adults, it can appear at any age – from infancy to much later in life. When it appears in adults, it's sometimes called Latent Autoimmune Diabetes in Adults (LADA), but it's still T1D at its core.
Risk Factors
The exact reason why someone develops T1D isn't fully understood, but scientists believe it's a combination of:
- Genetics: If you have a close family member (parent, sibling) with T1D, your risk is slightly higher. However, most people who develop T1D have no family history of the disease. It's not inherited in the same way as eye color.
- Environmental Triggers: Researchers think that certain environmental factors, like viruses (e.g., enteroviruses), might trigger the immune system attack in genetically susceptible individuals. This is still an area of active research.
- Geography: T1D is more common in some parts of the world than others, with Scandinavian countries having some of the highest rates.
It's crucial to remember that T1D is not contagious, and it's not caused by something you did or didn't do. It's an unpredictable immune system response.
Recognizing the Signs: Symptoms of Type 1 Diabetes
The symptoms of Type 1 Diabetes often appear suddenly and can be quite severe. They are usually a result of high blood sugar (hyperglycemia) and the body trying to get rid of excess glucose. Doctors often refer to the “4 Ts” as common early warning signs:
- Thirst (Polydipsia): Feeling very thirsty, even after drinking a lot. Your body tries to flush out excess sugar through urine, leading to dehydration.
- Toilet (Polyuria): Urinating a lot, more frequently than usual, including waking up at night to pee. This is the body's way of getting rid of extra sugar.
- Thin (Weight Loss): Losing weight without trying. Even though you might be eating more, your cells aren't getting glucose for energy, so the body starts burning fat and muscle instead.
- Tired (Fatigue): Feeling extremely tired and lethargic. Lack of energy in your cells makes you feel run down.
Other symptoms can include:
- Extreme hunger (Polyphagia): Even though you're eating, your cells are starving for energy.
- Blurred vision: High blood sugar can affect the tiny blood vessels in your eyes, causing temporary vision changes. For more detailed information, see Early Stage Diabetes Eye Symptoms.
- Frequent infections: Such as yeast infections or skin infections.
- Nausea and vomiting: Especially if blood sugar levels are very high, leading to a serious condition called Diabetic Ketoacidosis (DKA). It's vital to know the signs of DKA; you can learn more about its symptoms here: Diabetic Ketoacidosis Symptoms.
- Fruity-smelling breath: A sign of DKA, caused by chemicals called ketones building up in the blood.
If you notice these symptoms in yourself or someone you know, it's essential to seek medical attention immediately. Early diagnosis and treatment can prevent serious complications.
Diagnosis: How Doctors Confirm Type 1 Diabetes
Diagnosing Type 1 Diabetes usually involves a few simple blood tests. If symptoms suggest T1D, a doctor will typically order one or more of the following:
- Random Plasma Glucose (RPG) Test: This measures your blood sugar at any time. A level of 200 mg/dL (11.1 mmol/L) or higher, along with symptoms, suggests diabetes.
- Fasting Plasma Glucose (FPG) Test: This measures your blood sugar after you haven't eaten for at least 8 hours. A level of 126 mg/dL (7.0 mmol/L) or higher on two separate tests indicates diabetes.
- A1C Test (Glycated Hemoglobin Test): This test shows your average blood sugar level over the past 2-3 months. An A1C of 6.5% or higher indicates diabetes. For T1D, it's often much higher at diagnosis.
- Autoantibody Tests: These tests look for specific antibodies in your blood that attack the pancreas. Finding these antibodies (like GAD65, ICA, IA-2A, ZnT8A) confirms that the diabetes is autoimmune (Type 1) and not Type 2.
- C-peptide Test: This test measures how much C-peptide your body makes. C-peptide is released into the blood in equal amounts as insulin. A very low or undetectable C-peptide level suggests that your pancreas is producing little to no insulin, which is typical for T1D.
Once diagnosed, a person with T1D will begin working with an endocrinologist (a doctor specializing in hormones and diabetes) and a diabetes care team to create a personalized management plan.
Living with Type 1 Diabetes: Daily Management
Living with Type 1 Diabetes means taking on the role of your own pancreas. This requires continuous effort and attention to detail, but modern tools and knowledge make it much more manageable than in previous decades. The focus is on precision and automation.
1. Insulin Therapy: Your Lifeline
Since the body can't make its own insulin, external insulin is absolutely essential for survival. There are different types of insulin, each working at different speeds and durations:
- Rapid-acting insulin: Works quickly (5-15 minutes), peaks in 30-90 minutes, lasts 3-5 hours. Taken before meals.
- Short-acting insulin: Works in 30-60 minutes, peaks in 2-4 hours, lasts 5-8 hours. Taken before meals.
- Intermediate-acting insulin: Works in 1-2 hours, peaks in 4-12 hours, lasts 14-24 hours.
- Long-acting insulin (Basal insulin): Works in 1-2 hours, has no peak or a very flat peak, lasts up to 24 hours or longer. Provides a steady background dose of insulin.
How is insulin delivered?
- Multiple Daily Injections (MDI): Many people use insulin pens or syringes to inject insulin several times a day. This typically involves a long-acting insulin once or twice a day and rapid-acting insulin with meals and to correct high blood sugars.
- Insulin Pumps: These small, computerized devices deliver rapid-acting insulin continuously through a tiny tube (cannula) inserted under the skin. Pumps offer more flexibility and precision, mimicking the pancreas more closely. Many modern pumps are now part of “closed-loop” or “hybrid closed-loop” systems, often called Artificial Pancreas Systems. These systems connect a continuous glucose monitor (CGM) directly to an insulin pump, automatically adjusting insulin delivery based on real-time glucose readings. This technology has been a game-changer, significantly reducing the burden of manual adjustments.
2. Blood Sugar Monitoring: Knowing Your Numbers
Knowing your blood sugar levels is like knowing the speed of your car. It tells you if you need more or less insulin, or if you need to eat something.
- Fingerstick Blood Glucose Meters: These are traditional devices where you prick your finger to get a drop of blood and place it on a test strip. While still used, especially for calibration, they provide only a snapshot in time.
- Continuous Glucose Monitors (CGMs): This technology has revolutionized T1D management. A small sensor is inserted under the skin (usually on the arm or abdomen) and worn for 7-14 days. It continuously measures glucose levels in the interstitial fluid (fluid surrounding cells) and sends readings wirelessly to a receiver or smartphone app. CGMs provide real-time data, trend arrows (showing if glucose is rising or falling), and alarms for high or low levels. This allows for proactive adjustments and better control, helping individuals unlock a better life with diabetes.
3. Carbohydrate Counting and Diet: Fueling Your Body
Food plays a huge role in blood sugar management. Carbohydrates (carbs) are the main type of food that directly affects blood sugar.
- Carbohydrate Counting: This is a fundamental skill for people with T1D. It involves estimating the amount of carbohydrates in meals and snacks. Based on this count, and their individual insulin-to-carb ratio, they calculate how much rapid-acting insulin to take.
- Balanced Diet: While carb counting is essential, a healthy, balanced diet rich in fruits, vegetables, lean proteins, and whole grains is important for overall health. There's no specific “diabetic diet” that's universally prescribed for T1D; the focus is on managing carbs and eating nutritious foods.
- Meal Timing: Consistency in meal times and carb intake can help stabilize blood sugar, though modern insulin therapy and pump technology offer more flexibility than in the past.
4. Exercise and Physical Activity: Staying Active
Physical activity is beneficial for everyone, including people with T1D. It can improve insulin sensitivity (meaning the body uses insulin more effectively) and cardiovascular health. However, exercise can also significantly impact blood sugar levels.
- Monitoring is Key: Blood sugar needs to be closely monitored before, during, and after exercise.
- Adjustments: Insulin doses may need to be reduced, or extra carbohydrates consumed, to prevent low blood sugar (hypoglycemia) during or after activity.
- Hydration: Staying well-hydrated is always important, especially during exercise.
5. Managing Hypoglycemia and Hyperglycemia: The Ups and Downs
These are the two main challenges in day-to-day T1D management.
- Hypoglycemia (Low Blood Sugar): This occurs when blood sugar drops too low (typically below 70 mg/dL or 3.9 mmol/L). It can happen if too much insulin is taken, not enough food is eaten, or due to intense exercise.
- Symptoms: Shakiness, sweating, hunger, confusion, dizziness, irritability.
- Treatment: Eating or drinking 15 grams of fast-acting carbohydrates (e.g., glucose tablets, juice, regular soda) and rechecking blood sugar after 15 minutes. Severe hypoglycemia can lead to unconsciousness and requires glucagon.
- Hyperglycemia (High Blood Sugar): This occurs when blood sugar is too high (typically above 180 mg/dL or 10 mmol/L). It can happen if not enough insulin is taken, too many carbs are eaten, or due to stress, illness, or hormonal changes.
- Symptoms: Increased thirst, frequent urination, fatigue, blurred vision.
- Treatment: Taking extra insulin (a “correction dose”) and drinking water. If high blood sugar is left untreated, it can lead to complications like DKA.
“Living with Type 1 Diabetes is a marathon, not a sprint. It requires constant learning, adaptability, and a strong partnership with your healthcare team.” — A diabetes educator.
Challenges and Emotional Impact
Beyond the physical demands, living with Type 1 Diabetes carries a significant emotional and mental burden.
- Diabetes Burnout: The constant need for monitoring, counting, and decision-making can lead to fatigue, frustration, and a feeling of being overwhelmed. This is often called “diabetes burnout.”
- Mental Health: People with T1D are at a higher risk for depression, anxiety, and eating disorders. The pressure to maintain perfect control can be immense.
- Social Impact: Managing T1D can affect social activities, travel, and relationships, requiring open communication and understanding from others.
- Fear of Complications: The long-term risks associated with diabetes, such as nerve damage, kidney disease, heart disease, and vision problems, can be a constant source of worry. Regular check-ups and good management can significantly reduce these risks. Understanding the broad impact of diabetes mellitus can provide context for these concerns. You can read more about it here: Diabetes Mellitus.
It's crucial for individuals with T1D, and their families, to acknowledge these challenges and seek support from mental health professionals, support groups, and their diabetes care team.
Advancements and Future Outlook in T1D Management
The field of diabetes care is constantly evolving, and sees exciting progress.
- Artificial Pancreas Systems (Hybrid Closed-Loop): As mentioned, these systems are becoming more sophisticated and widely available. They use algorithms to predict glucose trends and adjust insulin delivery, freeing individuals from some of the constant manual decision-making. Future systems aim for full automation, requiring even less user input.
- Newer Insulins: Research continues into insulins that act even faster or last even longer, offering greater flexibility and better control.
- Smart Insulin Pens: These pens record insulin doses and times, often syncing with smartphone apps, to provide better data for management.
- Encapsulation and Beta Cell Regeneration: Scientists are actively researching ways to protect transplanted beta cells from the immune system or even to regenerate new insulin-producing cells in the body. While still in experimental stages, these avenues offer hope for a potential cure in the distant future.
- Immunotherapy: Research is also exploring therapies that could “retrain” the immune system to stop attacking beta cells, potentially preventing T1D in high-risk individuals or preserving remaining beta cells in newly diagnosed patients.
These advancements offer tremendous hope for improved quality of life and even a cure for Type 1 Diabetes.
Debunking Common Myths About Type 1 Diabetes
There are many misconceptions about diabetes, and T1D often gets confused with T2D. Let's set the record straight:
Myth 1: Type 1 Diabetes is caused by eating too much sugar or unhealthy foods.
- Truth: Absolutely false. T1D is an autoimmune disease. It's not caused by diet or lifestyle. Eating habits only become a factor after diagnosis, as they need to be managed to control blood sugar.
Myth 2: People with Type 1 Diabetes can “grow out of it.”
- Truth: T1D is a lifelong condition. Once the beta cells are destroyed, they don't regenerate naturally. Insulin therapy is required for life, unless a cure is found.
Myth 3: Type 1 Diabetes is less serious than Type 2 Diabetes.
- Truth: Both types of diabetes are serious and can lead to severe complications if not managed properly. T1D, however, is immediately life-threatening without insulin, as the body produces none.
Myth 4: People with Type 1 Diabetes can't eat sweets or carbohydrates.
- Truth: People with T1D can eat sweets and carbohydrates, but they must carefully count the carbs and take the appropriate amount of insulin to cover them. It's all about balance and management, not outright restriction.
Myth 5: Insulin is a cure for Type 1 Diabetes.
- Truth: Insulin is a life-sustaining treatment, but it is not a cure. It replaces the insulin the body can no longer make.
Myth 6: Only children get Type 1 Diabetes.
- Truth: While often diagnosed in childhood, T1D can develop at any age. It's essential to recognize the symptoms regardless of age.
Conclusion:
Type 1 Diabetes is a complex condition, but with the right knowledge, tools, and support, individuals can lead healthy, fulfilling lives. The landscape of T1D management is more advanced and hopeful than ever before, thanks to innovations like continuous glucose monitors, advanced insulin pumps, and the emerging artificial pancreas systems.
Understanding that T1D is an autoimmune condition, not a lifestyle choice, is crucial for both those living with it and their communities. By debunking myths, embracing education, and leveraging modern technology, we can foster a world where people with Type 1 Diabetes feel empowered, not limited, by their condition. If you or someone you know is experiencing symptoms, seek medical advice immediately. Early diagnosis and consistent management are the keys to thriving with Type 1 Diabetes.