Feeling overwhelmed by a Stage 2 hypertension treatment? You're not alone. High blood pressure, especially at this elevated level, can be a serious health concern, but the good news is that advancements in treatment are constantly evolving. We're seeing exciting breakthroughs that offer new hope and more effective ways to manage this condition.
This article will guide you through the latest innovations, from cutting-edge medications and device-based therapies to personalized lifestyle strategies and the power of technology, all designed to help you take control of your blood pressure and improve your health.
Explore Stage 2 Hypertension Treatment Options
Click on a category to learn about different treatment approaches for Stage 2 Hypertension in 2025.
Select a treatment category above to see details and breakthroughs for Stage 2 Hypertension in 2025.
Key Takeaways
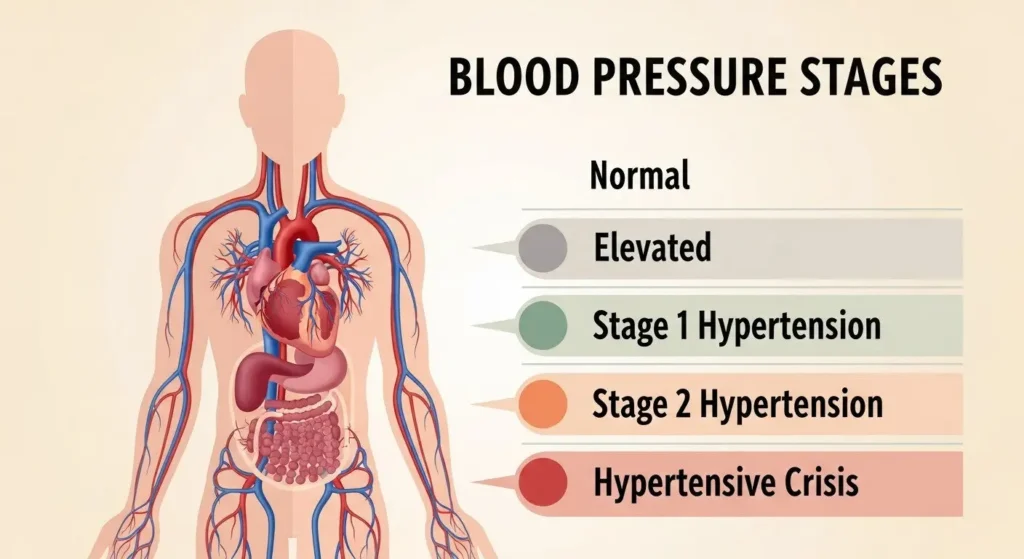
- Understanding Stage 2 Hypertension treatment is Crucial: It's defined by consistent blood pressure readings of 140/90 mmHg or higher and requires prompt, effective management to prevent serious health complications.
- New Medications Offer Targeted Relief: Novel drug classes and smarter combination therapies can lower blood pressure more effectively with fewer side effects.
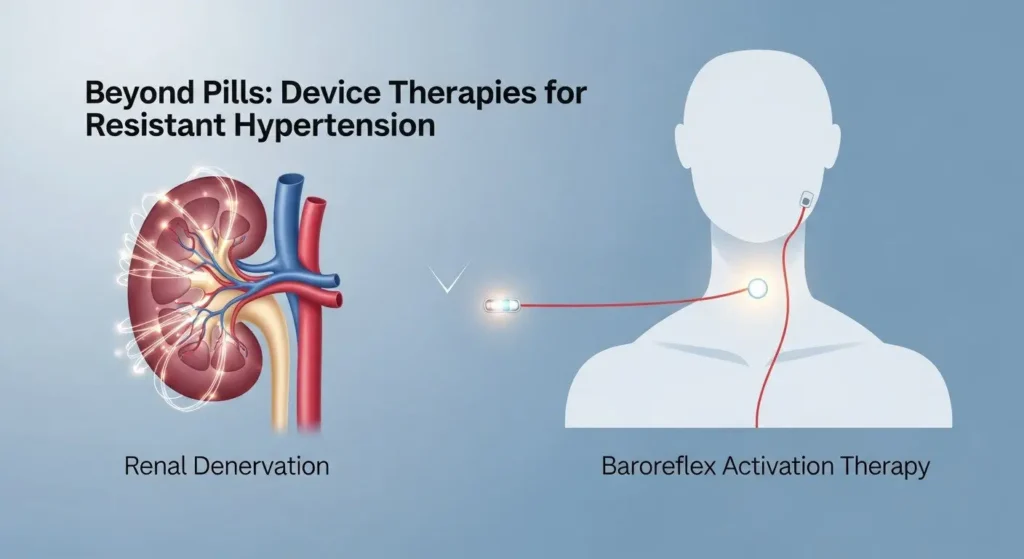
- Device-Based Therapies are Emerging: For those who struggle with medication, options like renal denervation and baroreflex activation therapy provide innovative, non-pharmacological ways to control blood pressure.
- Personalized Lifestyle & Technology are Game-Changers: Tailored nutrition plans, advanced exercise routines, stress management, remote monitoring, and AI-driven insights are making Stage 2 hypertension treatment more effective and accessible than ever.
- Proactive Management is Key: By understanding these breakthroughs and working closely with your healthcare team, you can achieve better blood pressure control and significantly improve your long-term health.
What is Stage 2 Hypertension treatment? Understanding the Stakes
Before we dive into the exciting breakthroughs, let's make sure we're all on the same page about what Stage 2 hypertension treatment means. When you get your blood pressure checked, you'll see two numbers:
- Systolic pressure (the top number): This measures the pressure in your arteries when your heart beats.
- Diastolic pressure (the bottom number): This measures the pressure in your arteries when your heart rests between beats.
According to the American Heart Association (AHA), Stage 2 hypertension treatment is diagnosed when your blood pressure consistently reads 140/90 mmHg or higher. This isn't just a slightly elevated reading; it's a significant indicator that your heart and blood vessels are working harder than they should be, and it increases your risk for serious health problems.
Why is Stage 2 Hypertension treatment a Big Deal?
Think of your blood vessels like pipes. If the pressure inside them is constantly too high, it puts a lot of strain on the pipes and the pump (your heart). Over time, this can lead to:
- Heart attack and stroke: High pressure damages arteries, making them stiff and narrow.
- Heart failure: Your heart has to work too hard and can become weakened.
- Kidney disease: High blood pressure can damage the delicate blood vessels in your kidneys.
- Vision loss: Tiny blood vessels in your eyes can be damaged.
- Peripheral artery disease: Affects blood flow to your limbs.
The good news is that Stage 2 hypertension is treatable, and with the right approach, you can significantly reduce these risks. That's why understanding the latest breakthroughs is so important!
The Foundation: Traditional Stage 2 Hypertension Treatment
Even with new breakthroughs, the foundation of Stage 2 hypertension treatment still rests on two main pillars: lifestyle changes and medication. These traditional approaches have been proven effective for decades and often serve as the first line of defense.
Lifestyle Changes: Your First and Most Powerful Tool
Before any medication, your doctor will likely recommend significant lifestyle adjustments. These are often the most effective ways to lower blood pressure naturally and can even reduce the need for medication for some individuals.
- Dietary Adjustments: The DASH (Dietary Approaches to Stop Hypertension) diet is often recommended. It focuses on:
- Eating plenty of fruits, vegetables, and whole grains.
- Including lean protein and low-fat dairy.
- Reducing saturated and trans fats, cholesterol, and especially sodium.
- Pull Quote: “Eating less salt is one of the quickest ways to see a drop in blood pressure.”
- Regular Physical Activity: Aim for at least 150 minutes of moderate-intensity aerobic exercise per week. This could be brisk walking, swimming, cycling, or dancing. Even short bursts of activity throughout the day add up! Want to know what cardio burns the most calories? Learn more about effective cardio workouts for weight loss.
- Weight Management: Losing even a small amount of weight can have a big impact on blood pressure. If you're overweight or obese, working towards a healthy weight is crucial. Maintaining a healthy weight also impacts other conditions, like Type 3 diabetes symptoms, which can be related to metabolic health.
- Limiting Alcohol and Quitting Smoking: Both alcohol (in excess) and smoking significantly raise blood pressure and damage blood vessels.
- Stress Reduction: Chronic stress can contribute to high blood pressure. Techniques like meditation, yoga, deep breathing exercises, and spending time in nature can help. 🧘♀️
- Adequate Sleep: Aim for 7-9 hours of quality sleep per night. Poor sleep can negatively impact blood pressure.
Medications: When Lifestyle Isn't Enough
For most people with Stage 2 hypertension, lifestyle changes alone aren't enough, and medication becomes necessary. There are several classes of drugs commonly used, often in combination:
- Diuretics (Water Pills): Help your body get rid of excess sodium and water, reducing blood volume.
- ACE Inhibitors and ARBs (Angiotensin Receptor Blockers): Relax blood vessels by blocking the formation or effects of a hormone that narrows them.
- Calcium Channel Blockers: Relax blood vessels and can slow your heart rate.
- Beta-Blockers: Reduce heart rate and the force of your heart's contractions.
- Alpha-Blockers: Relax the muscles in the blood vessel walls.
Often, doctors will start with one medication and then add others or switch to combination pills if blood pressure isn't controlled. For a deeper dive into various hypertension treatments, you can explore more options.
The Breakthroughs: New Medications and Smart Combinations
The landscape of medication for Stage 2 hypertension treatment is constantly evolving. We're seeing exciting developments that offer more targeted and effective ways to lower blood pressure, often with fewer side effects.
Novel Drug Classes: Beyond the Traditional
While ACE inhibitors and diuretics remain staples, researchers are exploring entirely new mechanisms to control blood pressure.
- Endothelin Receptor Antagonists (ERAs) for Specific Cases: While primarily used for pulmonary hypertension, new research is exploring ERAs with improved safety profiles for systemic hypertension, particularly in resistant cases. These drugs block endothelin, a powerful blood vessel constrictor.
- Aldosterone Synthase Inhibitors (ASIs): Aldosterone is a hormone that can raise blood pressure by increasing salt and water retention. ASIs work by directly blocking the enzyme that produces aldosterone, offering a more targeted approach than traditional aldosterone antagonists. Early results are promising for resistant hypertension.
- Renin Inhibitors (e.g., Aliskiren): Though not entirely new, there's renewed interest in optimizing their use and exploring combination therapies. These drugs block renin, an enzyme that starts the cascade leading to blood vessel constriction.
- Vaccines for Hypertension? (Future Outlook): This is still in early research phases, but scientists are exploring therapeutic vaccines that could train the immune system to produce antibodies against blood pressure-raising hormones. Imagine a shot that helps keep your blood pressure low for months! This is a fascinating prospect for the future.
Single-Pill Combination Therapies: Simplify Your Routine
One of the biggest challenges in managing Stage 2 hypertension treatment is medication adherence. Taking multiple pills at different times can be confusing and lead to missed doses. The trend is towards single-pill combinations (SPCs) that combine two or even three different blood pressure medications into one tablet.
Benefits of SPCs:
- Improved Adherence: Fewer pills mean it's easier to remember to take your medication.
- Enhanced Efficacy: Combining drugs with different mechanisms of action often leads to better blood pressure control than increasing the dose of a single drug.
- Reduced Side Effects: Often, lower doses of multiple drugs can be used, potentially reducing side effects compared to high doses of a single drug.
Example: A common SPC might combine an ACE inhibitor with a diuretic, or a calcium channel blocker with an ARB. Your doctor can help determine if an SPC is right for you.

Device-Based Therapies: Non-Drug Solutions
For some individuals with Stage 2 hypertension treatment, especially those with resistant hypertension (blood pressure that remains high despite taking three or more blood pressure medications, including a diuretic), device-based therapies offer a new frontier. These approaches use medical devices to help regulate blood pressure without daily pills.
1. Renal Denervation (RDN)
This therapy involves using radiofrequency energy or ultrasound to calm overactive nerves near the kidneys. These nerves play a role in regulating blood pressure. By reducing their activity, RDN can help lower blood pressure.
How it Works:
- A thin, flexible tube (catheter) is inserted into an artery, usually in the leg, and guided to the renal arteries (which supply blood to the kidneys).
- Energy is delivered to tiny nerves surrounding these arteries.
- This procedure is minimally invasive and typically done in a hospital setting.
Current Status: After years of research, RDN is gaining traction and becoming a more accessible option in various regions. It's particularly promising for patients who don't respond well to traditional medications or struggle with side effects. Clinical trials continue to refine patient selection and long-term outcomes.
2. Baroreflex Activation Therapy (BAT)
Baroreceptors are specialized nerve endings located in your carotid arteries (in your neck) that sense blood pressure changes and send signals to your brain to help regulate it. In BAT, a small device is implanted under the skin in the chest, similar to a pacemaker. A wire connects it to the carotid artery, where it delivers mild electrical pulses.
How it Works:
- These pulses stimulate the baroreceptors, tricking them into thinking blood pressure is higher than it is.
- This sends signals to the brain, which then responds by relaxing blood vessels and slowing the heart rate, thereby lowering blood pressure.
Current Status: BAT is also an option for resistant hypertension, offering another non-pharmacological pathway to control blood pressure. It's a more invasive procedure than RDN, but for the right patient, it can provide significant and sustained blood pressure reduction.
3. Arteriovenous Fistula Creation (for Dialysis Patients)
While not a direct hypertension treatment for everyone, for patients with end-stage renal disease on dialysis who also suffer from severe resistant hypertension, creating an arteriovenous fistula (a surgical connection between an artery and a vein) for dialysis access has been shown in some cases to paradoxically lower blood pressure. This is a highly specialized approach and not a general hypertension treatment, but it's an interesting medical observation.
Advanced Lifestyle Interventions: Personalizing Your Path
While the core principles of healthy living remain, 2025 brings more personalized and advanced approaches to lifestyle interventions, making them even more powerful tools in your Stage 2 hypertension treatment plan.
1. Precision Nutrition and Dietary Guidance
Forget one-size-fits-all diets. Today, nutrition plans are becoming highly individualized, considering your genetics, gut microbiome, and specific health needs.
- Genetic Testing for Dietary Response: Some tests can now provide insights into how your body processes sodium, caffeine, and certain fats, allowing for a truly tailored dietary approach.
- Gut Microbiome Optimization: Research increasingly links gut health to blood pressure regulation. Personalized dietary recommendations might include specific probiotics or prebiotics to foster a healthy gut flora.
- Advanced Nutrient Timing: Working with a registered dietitian, you can optimize when and what you eat to support blood pressure control throughout the day.
This personalized approach goes beyond just “eat your veggies” to “eat these veggies at this time because your body responds best to them.”
2. Tailored Exercise Prescriptions
Just like nutrition, exercise is becoming more precise. Instead of just “get active,” your doctor or a specialized exercise physiologist might recommend:
- High-Intensity Interval Training (HIIT): Short bursts of intense exercise followed by recovery periods can be highly effective for cardiovascular health and blood pressure, often in less time than traditional cardio.
- Strength Training Integration: Building muscle mass improves metabolism and can help with weight management, which indirectly benefits blood pressure.
- Mind-Body Exercises: Yoga, Tai Chi, and Pilates combine physical movement with breathwork and mindfulness, offering both physical and stress-reducing benefits.
- Activity Trackers and Wearables: These devices provide real-time feedback, helping you stay motivated and track your progress. Learn more about how various forms of cardio can help with weight loss.
3. Next-Level Stress Management and Mental Well-being
The link between stress and high blood pressure is undeniable. In 2025, stress management tools are becoming more sophisticated and accessible:
- Digital Therapeutics (DTx): Apps and online programs offering guided meditation, cognitive behavioral therapy (CBT) for stress, and mindfulness exercises.
- Biofeedback and Neurofeedback: These techniques help you learn to control physiological responses like heart rate and blood pressure by giving you real-time feedback on your body's functions.
- Mindfulness-Based Stress Reduction (MBSR): Structured programs that teach mindfulness techniques to manage stress, anxiety, and chronic pain, which can indirectly impact blood pressure.
4. The Role of Supplements (with Caution)
While no supplement can replace medication or lifestyle changes, some show promise for blood pressure support when used under medical supervision.
- Potassium: Helps balance sodium levels. Found in fruits and vegetables.
- Magnesium: Plays a role in blood vessel relaxation.
- Omega-3 Fatty Acids: May help reduce inflammation and improve blood vessel function.
- Vitamin D: Emerging research links Vitamin D deficiency to higher blood pressure. While it won't magically cure hypertension, ensuring adequate levels is important for overall health. You can explore topics like whether Vitamin D helps with weight loss and separate Vitamin D myths vs. facts for weight loss to understand its broader health implications.
Important Note: Always discuss any supplements with your doctor, as they can interact with medications or have side effects.
The Power of Technology: Monitoring and Personalized Insights
Technology is revolutionizing how we monitor and manage Stage 2 hypertension treatment, moving us towards more proactive and personalized care.
1. Remote Blood Pressure Monitoring
Gone are the days of only checking your blood pressure at the doctor's office. Smart blood pressure cuffs are now widely available, allowing you to:
- Track Readings at Home: Consistent home readings provide a more accurate picture of your average blood pressure, free from “white coat hypertension.”
- Share Data Instantly: Many devices sync with apps and can securely share data with your doctor, allowing them to adjust your treatment plan more quickly if needed.
- Receive Reminders: Apps can remind you to take readings and medication, improving adherence.
2. Artificial Intelligence (AI) and Machine Learning
AI is beginning to play a significant role in hypertension management:
- Predictive Analytics: AI can analyze vast amounts of patient data to predict who is at higher risk for uncontrolled hypertension or complications, allowing for earlier intervention.
- Personalized Treatment Recommendations: By analyzing your unique health profile (genetics, lifestyle, medication history), AI algorithms can suggest the most effective treatment combinations.
- Digital Health Coaches: AI-powered apps can act as virtual health coaches, providing personalized advice on diet, exercise, and stress management based on your data.
3. Wearable Devices and Continuous Monitoring
While not yet ready for continuous blood pressure monitoring, wearables are getting smarter:
- Heart Rate Variability (HRV): Some wearables track HRV, which can be an indicator of stress levels and overall cardiovascular health.
- Activity and Sleep Tracking: These metrics indirectly influence blood pressure and provide valuable data for lifestyle adjustments.
- Pull Quote: “Ttechnology isn't just a gadget; it's a partner in your health journey.”

Personalized Medicine: Tailoring Treatment to You
The future of Stage 2 hypertension treatment is increasingly personalized. This means moving away from a one-size-fits-all approach and towards treatments that are specifically designed for you.
1. Pharmacogenomics: Your Genes and Your Meds
Have you ever wondered why a medication works wonders for one person but has side effects or no effect on another? Pharmacogenomics is the study of how your genes affect your response to drugs.
- Predicting Drug Response: Genetic tests can reveal how your body metabolizes certain medications (e.g., how quickly you break them down). This can help your doctor choose the most effective drug at the right dose, reducing trial-and-error.
- Minimizing Side Effects: By knowing how you might react to a drug, your doctor can avoid medications that are likely to cause adverse effects for you.
This field is rapidly expanding and pharmacogenomic testing is becoming more integrated into prescribing practices for conditions like hypertension.
2. Biomarkers and Advanced Diagnostics
Beyond standard blood tests, new biomarkers are being identified that can provide deeper insights into the underlying causes of your hypertension.
- Inflammatory Markers: Chronic inflammation can contribute to high blood pressure. Identifying specific inflammatory markers can guide treatment.
- Endothelial Function Tests: These tests assess the health and function of the inner lining of your blood vessels, which is critical for blood pressure regulation.
- Hormone Panels: More comprehensive checks of hormones involved in blood pressure control (like aldosterone, renin, cortisol) can pinpoint specific imbalances.
These advanced diagnostics help create a more precise picture of your condition, leading to more targeted and effective treatment plans.
Managing Co-Existing Conditions: A Holistic View
Stage 2 hypertension treatment rarely exists in isolation. It often co-occurs with other health issues, and a holistic approach that manages all conditions simultaneously is crucial for overall health and blood pressure control.
1. Diabetes Management
High blood pressure and diabetes are often “partners in crime,” significantly increasing the risk of heart disease, kidney disease, and stroke.
- Integrated Treatment Plans: If you have both, your doctor will choose medications that benefit both conditions. For example, some blood pressure medications also protect the kidneys, which is vital for people with diabetes.
- Blood Sugar Control: Keeping blood sugar levels in check is critical. High blood sugar can damage blood vessels, making hypertension harder to control.
- Dietary Synergy: Diets recommended for hypertension (like DASH) are often beneficial for diabetes as well. It's about making smart choices for both.
- It's important to be aware of the connection between metabolic health and conditions like Type 3 diabetes symptoms, which highlights the importance of comprehensive care.
2. Weight Loss and Metabolic Health
Obesity is a major risk factor for hypertension. Losing weight, even a modest amount, can significantly lower blood pressure.
- Personalized Weight Loss Strategies: Beyond diet and exercise, new approaches include:
- GLP-1 Receptor Agonists: Medications like semaglutide and tirzepatide, originally for diabetes, are now also approved for weight loss and have shown cardiovascular benefits, including blood pressure reduction.
- Metabolic Surgery: For severe obesity, bariatric surgery can lead to significant and sustained weight loss, often resolving hypertension.
- Addressing Nutritional Deficiencies: Sometimes, seemingly unrelated factors can play a role. For instance, questions arise about whether Vitamin D helps with weight loss and understanding the Vitamin D and weight loss myths vs. facts can be part of a comprehensive nutritional plan to support metabolic health.
3. Cholesterol Management
High cholesterol often accompanies hypertension, further increasing cardiovascular risk.
- Statin Therapy: These medications are effective in lowering LDL (“bad”) cholesterol and are often prescribed alongside blood pressure medications.
- Lifestyle Synergy: The same healthy diet and exercise that help blood pressure also benefit cholesterol levels.
By tackling all these conditions together, you create a more powerful defense against serious health complications.
Empowering Yourself: What You Can Do Now
The breakthroughs in Stage 2 hypertension treatment are exciting, but your active participation is the most important factor in your success. Here’s how you can empower yourself:
- Be Proactive with Your Healthcare Team:
- Regular Check-ups: Don't miss your appointments. Regular monitoring is key.
- Open Communication: Discuss all your symptoms, concerns, and lifestyle habits honestly with your doctor. Ask questions about new treatments you've read about.
- Medication Adherence: Take your medications exactly as prescribed. If you have side effects, tell your doctor; don't just stop taking them.
- Team Approach: Consider working with a team that might include a cardiologist, a registered dietitian, and an exercise physiologist.
- Embrace Lifestyle Changes as Medicine:
- Consistency is Key: Make healthy eating and regular activity non-negotiable parts of your daily routine. Small, consistent changes add up to big results.
- Track Your Progress: Use journals, apps, or wearables to monitor your diet, exercise, and stress levels. Seeing your progress can be a huge motivator.
- Educate Yourself: The more you understand your condition and the available treatments, the better equipped you'll be to make informed decisions.
- Utilize Technology Wisely:
- Home Blood Pressure Monitoring: Invest in a reliable monitor and use it regularly. Share the data with your doctor.
- Health Apps: Explore reputable apps for medication reminders, diet tracking, exercise guidance, or stress management.
- Advocate for Yourself:
- If you feel your current treatment isn't working, or if you're interested in exploring new options like device therapies or pharmacogenomic testing, don't hesitate to discuss it with your doctor. You are your own best advocate.
The Future is Bright: Hope for Better Control
Looking ahead, the landscape of Stage 2 hypertension treatment is filled with optimism. From highly targeted medications and innovative device-based therapies to the power of personalized medicine and smart technology, there are more tools than ever before to help you achieve and maintain healthy blood pressure.
Remember, managing Stage 2 hypertension treatment is a journey, not a destination. It requires ongoing effort, but with these new breakthroughs and your commitment, you can live a healthier, longer life. Stay informed, stay proactive, and work closely with your healthcare providers to leverage these incredible advancements for your well-being. Your heart will thank you!