Living with nonbacterial prostatitis can be a real challenge. It's a condition that affects many men, causing discomfort and pain, but it often doesn't respond to traditional antibiotics because, well, there's no bacterial infection to fight! If you're experiencing ongoing pelvic pain, urinary issues, or general discomfort in the prostate area, you're not alone. This often-misunderstood condition, also known as Chronic Pelvic Pain Syndrome (CPPS), can significantly impact your quality of life.
The good news? Many men find relief and better health by exploring natural and holistic approaches. In this comprehensive guide, we'll dive deep into understanding nonbacterial prostatitis and explore a wide range of natural strategies you can use to manage your symptoms, improve your well-being, and take control of your health journey. From dietary changes and herbal remedies to lifestyle adjustments and stress management techniques, we'll cover practical steps you can take. Let's get started on your path to feeling better! 🌱
Key Takeaways
- Understand the Condition: Nonbacterial prostatitis (Chronic Pelvic Pain Syndrome) causes pelvic pain and urinary issues without a bacterial infection, making traditional antibiotics ineffective.
- Embrace Anti-Inflammatory Foods: A diet rich in fruits, vegetables, whole grains, and healthy fats can reduce inflammation and support prostate health.
- Explore Natural Supplements: Herbal remedies like Saw Palmetto, Quercetin, and Rye Grass Flower Pollen Extract, along with vital nutrients like Zinc, can offer symptom relief.
- Prioritize Lifestyle Changes: Stress management (meditation, yoga), regular exercise, and avoiding irritants are crucial for reducing pain and improving overall well-being.
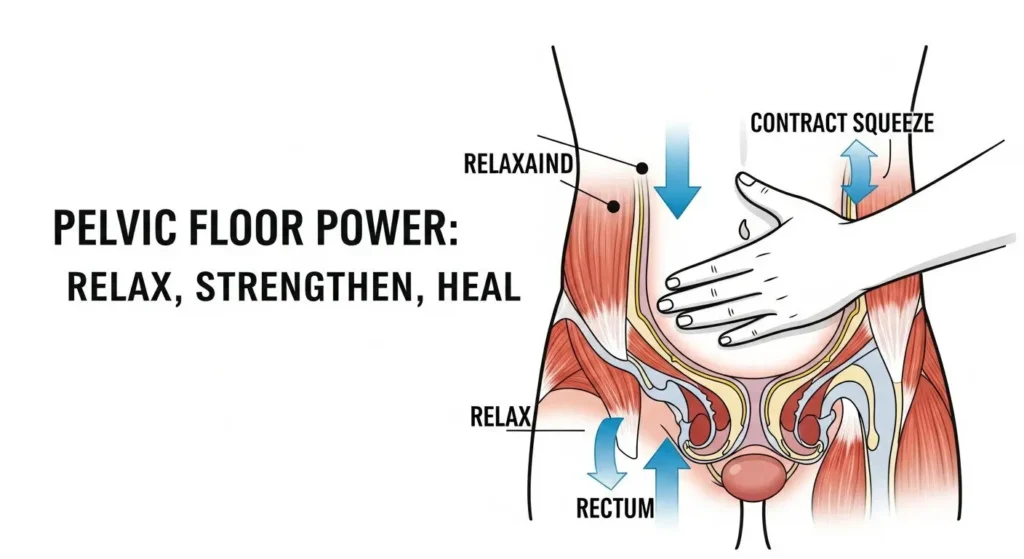
- Consider Pelvic Floor Therapy: Strengthening and relaxing pelvic floor muscles can significantly alleviate symptoms for many men with nonbacterial prostatitis.
What is Nonbacterial Prostatitis?
Imagine a small, walnut-sized gland located just below your bladder. That's your prostate. It plays an important role in the male reproductive system, producing fluid that nourishes and transports sperm. Sometimes, this gland can become inflamed or irritated, leading to a condition called prostatitis.
There are different types of prostatitis, and it's important to know the difference:
- Acute Bacterial Prostatitis: This is a sudden, severe bacterial infection of the prostate. It causes clear symptoms like fever, chills, body aches, and painful urination. It's usually treated with antibiotics.
- Chronic Bacterial Prostatitis: This is a recurring bacterial infection that causes milder but persistent symptoms, often after an acute infection. It also responds to antibiotics.
- Asymptomatic Inflammatory Prostatitis: This type shows inflammation of the prostate, but you don't feel any symptoms. It's usually discovered when testing for other conditions.
- Nonbacterial Prostatitis (Chronic Pelvic Pain Syndrome – CPPS): This is the focus of our guide. It's characterized by ongoing pelvic pain and urinary problems, but no bacterial infection is found. This means antibiotics won't help, which can be frustrating for many men seeking relief.
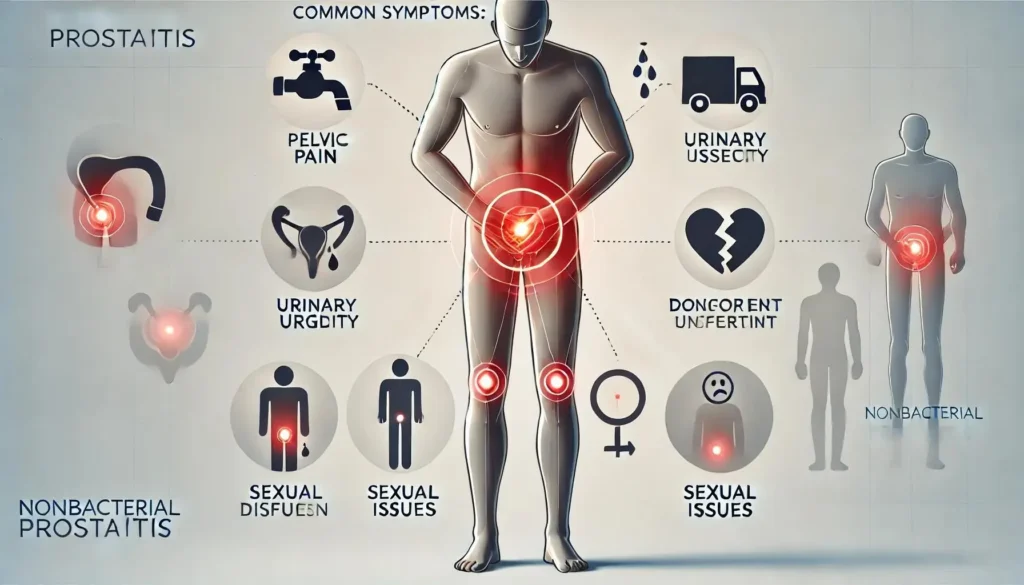
Symptoms of Nonbacterial Prostatitis
The symptoms of nonbacterial prostatitis can vary from person to person, but they often include:
- Pain: This is the most common symptom. It can be felt in the lower abdomen, groin, penis, testicles, lower back, or even between the scrotum and anus (perineum). The pain might be dull, aching, or sharp.
- Urinary Problems: You might experience frequent urges to pee, pain or burning during urination, difficulty starting or stopping urination, or a weak urine stream.
- Sexual Dysfunction: Pain during or after ejaculation, or a decreased sex drive, can also occur.
- Other Symptoms: Some men report fatigue, general discomfort, or even flu-like symptoms, though these are less common than with bacterial forms.
What Causes It?
This is the tricky part! Unlike bacterial prostatitis, where germs are the clear culprits, the exact cause of nonbacterial prostatitis is often unknown. This is why it's also called Chronic Pelvic Pain Syndrome (CPPS) – it highlights the pain aspect without pinning it to a specific infection.
However, doctors and researchers believe several factors might contribute to CPPS:
- Nerve Problems: Irritation or damage to the nerves in the pelvic area can send pain signals to the brain, even if there's no direct injury.
- Muscle Tension: Tight or spasming pelvic floor muscles can lead to chronic pain. Think of it like a muscle cramp that just won't go away.
- Stress and Psychological Factors: High stress levels, anxiety, and depression can worsen pain symptoms and even trigger flare-ups. The mind-body connection is very strong here.
- Immune System Issues: Sometimes, the body's immune system might mistakenly attack healthy cells, causing inflammation.
- Chemical Irritation: Urine refluxing into the prostate ducts could potentially cause irritation.
- Past Infections or Injuries: A previous infection or injury in the pelvic area might set the stage for chronic pain later on.
- Lifestyle Factors: Certain habits, like prolonged sitting or dehydration, might contribute to symptoms.
Diagnosing Nonbacterial Prostatitis
Diagnosing nonbacterial prostatitis usually involves ruling out other conditions. Your doctor will likely:
- Ask about your symptoms and medical history: They'll want to know when your pain started, what it feels like, and what makes it better or worse.
- Perform a physical exam: This typically includes a digital rectal exam (DRE) to check the prostate for tenderness or swelling.
- Conduct urine tests: This is crucial to check for bacteria and rule out a urinary tract infection (UTI).
- Perform semen analysis: This can also help rule out bacterial infections.
- Order other tests: Sometimes, blood tests, cystoscopy (looking inside the bladder with a tiny camera), or imaging tests (like an ultrasound or MRI) might be used to check for other problems.
The key takeaway is that if no bacteria are found, but you still have prostate-like symptoms, a diagnosis of nonbacterial prostatitis or CPPS is often made.
Why Consider Natural Approaches?
When faced with a condition that doesn't respond to standard treatments like antibiotics, it's natural to look for other solutions. This is where natural and holistic approaches shine. They offer a way to manage symptoms, reduce discomfort, and improve your overall quality of life, often with fewer side effects than some conventional medications.
Here's why many men turn to natural methods for nonbacterial prostatitis:
- Addressing the Root Cause (Holistically): Since the exact cause isn't always clear, natural approaches aim to support the body's healing processes, reduce inflammation, manage stress, and improve muscle function – all factors believed to contribute to CPPS.
- Fewer Side Effects: Many natural remedies, especially dietary and lifestyle changes, have minimal to no side effects compared to pharmaceutical drugs.
- Empowerment: Taking an active role in your health through natural methods can be empowering. You're making conscious choices to improve your well-being.
- Complementary Care: Natural approaches aren't always meant to replace conventional medicine but can work alongside it. Always discuss these options with your doctor.
- Overall Health Benefits: Many natural strategies, like eating better and reducing stress, benefit not just your prostate but your entire body and mind.
“Taking a natural path for nonbacterial prostatitis isn't about ignoring medical advice; it's about adding powerful, supportive tools to your health toolkit.”
Dietary Changes for Prostate Health
What you eat plays a huge role in your body's inflammation levels and overall health, including your prostate. Making smart food choices can significantly impact your symptoms. Think of your diet as a powerful tool to calm inflammation and support healing.
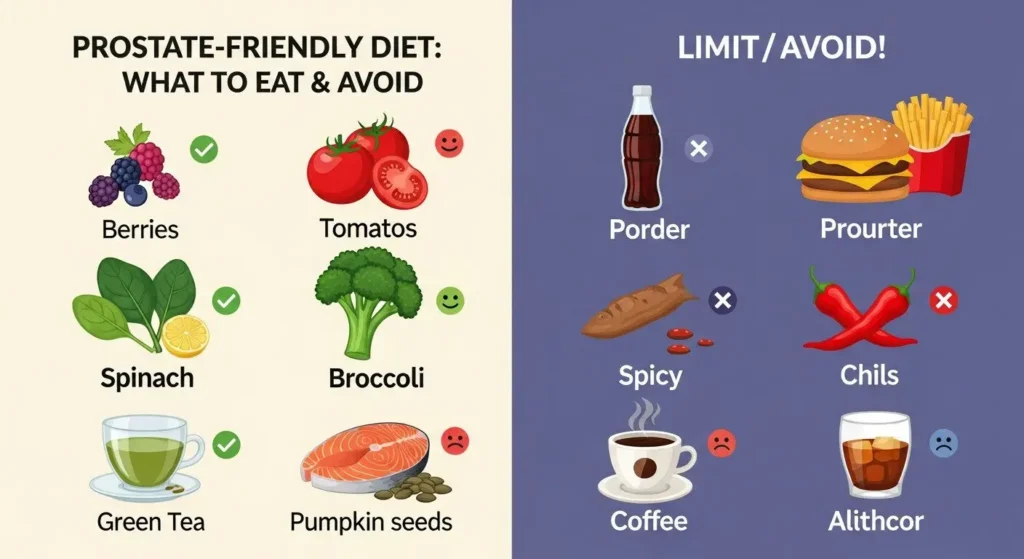
Anti-Inflammatory Foods to Embrace
Focus on foods that are rich in antioxidants, vitamins, and minerals, which can help reduce inflammation and protect your cells.
- Fruits and Vegetables: Aim for a rainbow of colors! Berries, cherries, oranges, spinach, kale, broccoli, tomatoes (especially cooked, for lycopene), and bell peppers are packed with inflammation-fighting compounds.
- Pro-Tip: Lycopene, found in cooked tomatoes, is particularly beneficial for prostate health.
- Whole Grains: Choose brown rice, quinoa, oats, and whole-wheat bread over refined grains. They provide fiber and nutrients that support gut health and reduce inflammation.
- Healthy Fats: Incorporate omega-3 fatty acids found in fatty fish (salmon, mackerel, sardines), flaxseeds, chia seeds, and walnuts. Olive oil and avocados are also great sources of healthy fats.
- Lean Proteins: Opt for plant-based proteins like beans, lentils, and tofu, or lean animal proteins like chicken and turkey.
- Nuts and Seeds: Almonds, walnuts, pumpkin seeds, and sunflower seeds are rich in zinc and other prostate-friendly nutrients. Pumpkin seeds, in particular, are often recommended.
- Green Tea: Known for its powerful antioxidants, especially catechins, which have anti-inflammatory properties.
Foods to Limit or Avoid
Certain foods can trigger or worsen inflammation and irritate the bladder and prostate. Try to reduce or eliminate these from your diet:
- Processed Foods: Sugary snacks, fast food, and highly processed meals often contain unhealthy fats, sugar, and artificial ingredients that promote inflammation.
- Red Meat and Processed Meats: High consumption of red meat (especially grilled or well-done) and processed meats (bacon, sausages) has been linked to inflammation and prostate issues.
- Spicy Foods: For many men with prostatitis, spicy foods can irritate the bladder and prostate, leading to increased pain and urinary urgency.
- Caffeine: Coffee, tea (except green tea), and energy drinks can act as bladder irritants. Try reducing your intake or switching to decaf.
- Alcohol: Alcohol can irritate the bladder and prostate, and some men find it worsens their symptoms. Limit or avoid it, especially during flare-ups.
- Acidic Foods: Some highly acidic foods, like citrus fruits or vinegar, might irritate some individuals. Pay attention to how your body reacts.
- Dairy Products: For some, dairy can be inflammatory. Consider a trial period without dairy to see if symptoms improve.
Hydration is Key!
Drinking plenty of water throughout the day is super important. It helps flush out your urinary system and can prevent urine from becoming too concentrated, which might irritate the bladder. Aim for at least 8 glasses of water daily.
Herbal Remedies and Supplements
Beyond diet, several natural supplements and herbal remedies have shown promise in helping manage nonbacterial prostatitis. These often work by reducing inflammation, supporting prostate function, or relaxing muscles.
Important Note: Always talk to your doctor before adding any new supplements to your routine, especially if you're taking other medications. Some supplements can interact with drugs or aren't suitable for everyone.
Let's look at some popular options:
1. Saw Palmetto (Serenoa repens)
This is perhaps one of the most well-known herbs for prostate health. Saw Palmetto extract is believed to help with urinary symptoms often associated with an enlarged prostate (BPH), but some studies also suggest it might have anti-inflammatory properties beneficial for prostatitis. It's thought to work by influencing hormone levels and reducing inflammation in the prostate.
- How it helps: May reduce inflammation, improve urinary flow.
- Dosage: Typically 160-320 mg daily, but follow product instructions or doctor's advice.
- Learn More: You can explore more about effective prostate supplements and their benefits by reading our guide on The Most Effective Prostate Supplements Reviewed for 2025.
2. Quercetin
Quercetin is a powerful antioxidant flavonoid found in many fruits, vegetables, and grains, such as apples, onions, and berries. It's known for its strong anti-inflammatory and pain-relieving properties, making it a popular choice for CPPS.
- How it helps: Reduces inflammation, acts as an antioxidant, may relieve pain.
- Dosage: Often 500 mg twice a day, sometimes combined with bromelain for better absorption.
3. Rye Grass Flower Pollen Extract (Cernilton)
This extract is a unique supplement that has been studied specifically for prostatitis symptoms. It's believed to help reduce inflammation, relax smooth muscles in the urinary tract, and decrease swelling in the prostate.
- How it helps: Anti-inflammatory, muscle relaxation, reduces swelling.
- Dosage: Varies, often around 300-500 mg daily.
4. Pygeum (Prunus africana)
Derived from the bark of the African plum tree, Pygeum has been traditionally used to treat urinary problems. It contains compounds that may help reduce inflammation, decrease prostate swelling, and improve urinary flow.
- How it helps: Anti-inflammatory, reduces swelling, improves urinary function.
- Dosage: Typically 50-100 mg daily.
5. Beta-Sitosterol
A plant sterol found in many plant foods, Beta-Sitosterol is often used for BPH symptoms. It may help reduce inflammation and improve urinary flow by reducing swelling in the prostate.
- How it helps: Anti-inflammatory, improves urinary symptoms.
- Dosage: Often 60-120 mg daily.
6. Zinc
Zinc is an essential mineral that plays a vital role in immune function and prostate health. Low zinc levels have been linked to prostate issues. Supplementing with zinc may help support prostate health and reduce inflammation.
- How it helps: Supports immune system, crucial for prostate health, anti-inflammatory.
- Dosage: Typically 15-30 mg daily, but be careful not to exceed safe limits as too much zinc can be harmful.
7. Magnesium
Magnesium is a mineral involved in over 300 bodily functions, including muscle relaxation and nerve function. For nonbacterial prostatitis, it might help by relaxing tight pelvic floor muscles and reducing nerve-related pain.
- How it helps: Muscle relaxation, nerve support, pain reduction.
- Dosage: 200-400 mg daily, often taken in citrate or glycinate forms for better absorption.
Considering Combination Supplements
Many men find success with combination supplements that blend several of these beneficial ingredients. Products like ProstaVive are designed to provide a comprehensive approach to prostate health by combining ingredients like Saw Palmetto, Beta-Sitosterol, Zinc, and other botanicals. If you're looking for a natural solution, understanding how these ingredients work together can be very helpful. You can learn more about how ProstaVive is tackling prostate problems head-on and get a deeper understanding of ProstaVive as a natural solution for prostate health. For a broader perspective on choosing the right supplement, check out our Guide to Prostate Supplements: Understanding and Your Choice.
Lifestyle Adjustments
Beyond diet and supplements, your daily habits and how you manage stress can significantly impact your nonbacterial prostatitis symptoms. Making small, consistent changes can lead to big improvements over time.
1. Stress Management
Stress is a huge trigger for many chronic pain conditions, including CPPS. When you're stressed, your muscles can tense up (including your pelvic floor muscles!), and your body's pain perception can increase. Finding healthy ways to manage stress is crucial.
- Mindfulness and Meditation: Even 10-15 minutes a day can make a difference. Apps like Calm or Headspace can guide you.
- Deep Breathing Exercises: Simple deep belly breathing can calm your nervous system. Inhale slowly through your nose, letting your belly rise, then exhale slowly through your mouth.
- Yoga or Tai Chi: These practices combine gentle movement, breathing, and mindfulness, which can be very effective for relaxing muscles and reducing stress.
- Spend Time in Nature: A walk in a park or forest can be incredibly calming. 🌳
- Hobbies: Engage in activities you enjoy to take your mind off pain and stress.
2. Regular Exercise (Gentle is Key!)
While intense exercise might sometimes worsen symptoms, regular, gentle physical activity can be very beneficial.
- Walking: A simple daily walk can improve circulation, reduce stress, and keep your body moving without putting strain on the pelvic area.
- Swimming: This low-impact exercise is excellent for overall fitness and doesn't put pressure on the perineum.
- Stretching: Gentle stretches for the hips, lower back, and glutes can help release tension that might be contributing to pelvic pain.
- Avoid High-Impact or Prolonged Sitting: Activities that put direct pressure on the perineum, like long-distance cycling or prolonged sitting on hard surfaces, can aggravate symptoms for some men. If you must sit for long periods, take frequent breaks to stand and stretch, and consider a special cushion designed to relieve pressure.
3. Heat Therapy
Applying gentle heat to the pelvic area can help relax tense muscles and relieve pain.
- Warm Baths: Soaking in a warm bath, perhaps with Epsom salts, can be very soothing.
- Heating Pads: A heating pad placed on the lower abdomen or lower back can provide localized relief.
4. Biofeedback
Biofeedback is a technique where you learn to control bodily functions, like muscle tension, that are usually involuntary. With the help of sensors, you get real-time feedback on your muscle activity, allowing you to learn how to relax tight pelvic floor muscles. This can be particularly useful for CPPS related to muscle tension.
5. Acupuncture
Acupuncture, a traditional Chinese medicine technique, involves inserting thin needles into specific points on the body. Many men with CPPS report significant pain relief and improved urinary symptoms with acupuncture, as it can help reduce inflammation and modulate pain signals.
6. Avoid Irritants and Maintain Good Hygiene
- Tight Clothing: Avoid tight underwear or pants that can put pressure on the perineal area and restrict blood flow.
- Caffeine and Alcohol: As mentioned in the diet section, these can irritate the bladder and prostate.
- Sexual Activity: While some men find sexual activity triggers pain, others find it helps. Pay attention to your body and discuss any concerns with your doctor.
- Regular Bowel Movements: Constipation can put pressure on the prostate. Ensure a diet rich in fiber and stay hydrated.
Pelvic Floor Therapy
For many men with nonbacterial prostatitis, the root of their pain lies in tight, dysfunctional, or spasming pelvic floor muscles. These muscles support your bladder and bowels, and if they're not working correctly, they can cause a lot of discomfort. This is where pelvic floor physical therapy comes in.
The Importance of Pelvic Floor Muscles
Your pelvic floor is like a hammock of muscles at the base of your pelvis. It plays a role in:
- Supporting your organs (bladder, bowel)
- Controlling urination and bowel movements
- Sexual function
When these muscles are too tight, weak, or uncoordinated, they can contribute to pelvic pain, urinary issues, and even sexual dysfunction, mimicking prostatitis symptoms.
Working with a Pelvic Floor Physical Therapist
A specialized pelvic floor physical therapist can be a game-changer. They will:
- Assess Your Muscles: They'll perform an internal and external examination to identify tight spots, trigger points, and areas of weakness or dysfunction.
- Teach Relaxation Techniques: Often, the first step is learning how to relax these muscles, not just strengthen them. Techniques might include diaphragmatic breathing, stretching, and myofascial release.
- Guide You Through Exercises:
- Reverse Kegels: Instead of squeezing, you learn to gently push down and relax your pelvic floor, like you're starting the flow of urine. This helps release tension.
- Stretching: Specific stretches for the hips, glutes, and inner thighs can indirectly help relax pelvic floor muscles.
- Provide Manual Therapy: The therapist might use hands-on techniques to release trigger points and tightness in your pelvic floor and surrounding muscles.
- Offer Biofeedback: Using special equipment, they can help you visualize your muscle activity, making it easier to learn how to control and relax your pelvic floor.
“Pelvic floor therapy isn't just about Kegels; it's about re-educating your muscles to function properly, often starting with relaxation.”
Kegel Exercises (With Caution!)
While Kegel exercises (squeezing and lifting the pelvic floor) are often recommended for pelvic health, they can sometimes worsen symptoms in men with tight pelvic floor muscles. If your muscles are already tense, strengthening them further might increase pain. This is why working with a therapist to determine if Kegels are right for you, and how to do them correctly, is so important. They can teach you how to properly engage and, more importantly, relax these muscles.
Understanding Your Triggers
One of the most powerful things you can do in your natural management journey is to become a detective of your own body. What makes your symptoms better? What makes them worse? Identifying your personal triggers can help you avoid flare-ups and find more consistent relief.
Consider keeping a symptom diary for a few weeks in 2025. Jot down:
- What you eat and drink: Note any spicy foods, caffeine, or alcohol.
- Your stress levels: Were you particularly stressed today?
- Your activity levels: Did you sit for a long time? Did you exercise?
- Your pain levels and location: Rate your pain on a scale of 1-10.
- Urinary symptoms: Frequency, urgency, pain.
- Bowel movements: Any constipation?
Over time, you might start to see patterns. For example, you might notice that a particularly spicy meal or a stressful day at work consistently leads to increased pelvic pain. This information is invaluable for tailoring your natural management plan.
When to See a Doctor
While natural approaches can be incredibly effective, it's crucial to remember that they are complementary to, not a replacement for, professional medical care. Always maintain open communication with your doctor.
You should definitely see your doctor if:
- Your symptoms suddenly worsen.
- You develop new symptoms like fever, chills, nausea, or vomiting. These could indicate an infection that requires immediate medical attention.
- You see blood in your urine or semen.
- You experience severe or debilitating pain.
- Your current natural strategies aren't providing enough relief after a consistent effort.
- You have concerns about any new supplement or treatment you're considering.
Your doctor can help ensure you have the correct diagnosis, rule out other conditions (like prostate cancer), and guide you on the safest and most effective treatment path, which might include a combination of conventional and natural therapies.
Holistic Approach to Wellness
Managing nonbacterial prostatitis naturally isn't just about targeting the prostate; it's about embracing a holistic approach to your entire well-being. When your whole body is healthier, it's better equipped to heal and manage chronic conditions.
- Prioritize Sleep: Quality sleep is vital for your body's repair processes and for managing pain. Aim for 7-9 hours of restful sleep each night. Create a relaxing bedtime routine and ensure your sleep environment is dark, quiet, and cool.
- Mental Health Support: Living with chronic pain can take a toll on your mental health. Don't hesitate to seek support from a therapist or counselor if you're struggling with anxiety, depression, or the emotional burden of your condition.
- Maintain a Healthy Weight: Excess body weight can contribute to inflammation and put additional strain on your body. Achieving and maintaining a healthy weight through diet and exercise can significantly improve overall health and potentially alleviate symptoms. If you're looking for support in your weight loss journey, you might find insights in Liv Pure Reviews: What to Expect When You Try It.
- Regular Check-ups: Continue with your regular doctor's appointments and screenings to monitor your overall health and address any other potential issues.
By taking care of your body and mind as a whole, you create the best environment for healing and long-term relief from nonbacterial prostatitis.
Conclusion
Navigating the complexities of nonbacterial prostatitis can be a long and sometimes frustrating journey. However, by embracing a proactive and natural approach, you can find significant relief and improve your quality of life and beyond. Remember, this isn't a quick fix, but a commitment to sustainable health.
From making conscious dietary choices to incorporating powerful herbal supplements, managing stress, adopting beneficial lifestyle habits, and exploring targeted therapies like pelvic floor physical therapy, you have a wide array of tools at your disposal. The key is patience, consistency, and listening to your body.
Always remember the importance of working closely with your healthcare provider. They can offer guidance, confirm your diagnosis, and ensure that your natural management plan complements any conventional treatments. By combining medical expertise with the wisdom of natural healing, you can build a comprehensive strategy to effectively manage nonbacterial prostatitis and reclaim your comfort and well-being.