Nearly 37 million people in the United States have diabetes, with many unaware they have it. Understanding type 2 vs type 1 diabetes is key for better care. Type 1 diabetes occurs when the body's immune system attacks the cells that make insulin, making it an autoimmune disease. Type 2 diabetes happens when the body's cells don't respond well to insulin, and the pancreas can't make enough to meet the body's needs.

Understanding Type 2 Vs Type 1 Diabetes
Diabetes mellitus is a long-term condition with high blood sugar levels. It can lead to serious health problems if not managed. In the United States, it affects millions of people.
What is Diabetes Mellitus?
Diabetes mellitus is a metabolic disorder. It happens when the body can't make enough insulin or use it well. Insulin helps glucose get into cells for energy.
The Role of Insulin in the Body
Insulin, made by the pancreas, is key to controlling blood sugar. It helps cells take in glucose, lowering blood sugar. In diabetes, the body either doesn't make enough insulin or its cells don't respond to it.
Prevalence and Impact in the United States
Diabetes is widespread in the United States, with type 2 being more common than type 1. Millions of Americans live with diabetes, diagnosed or undiagnosed. This shows the importance of being aware and managing the condition well.
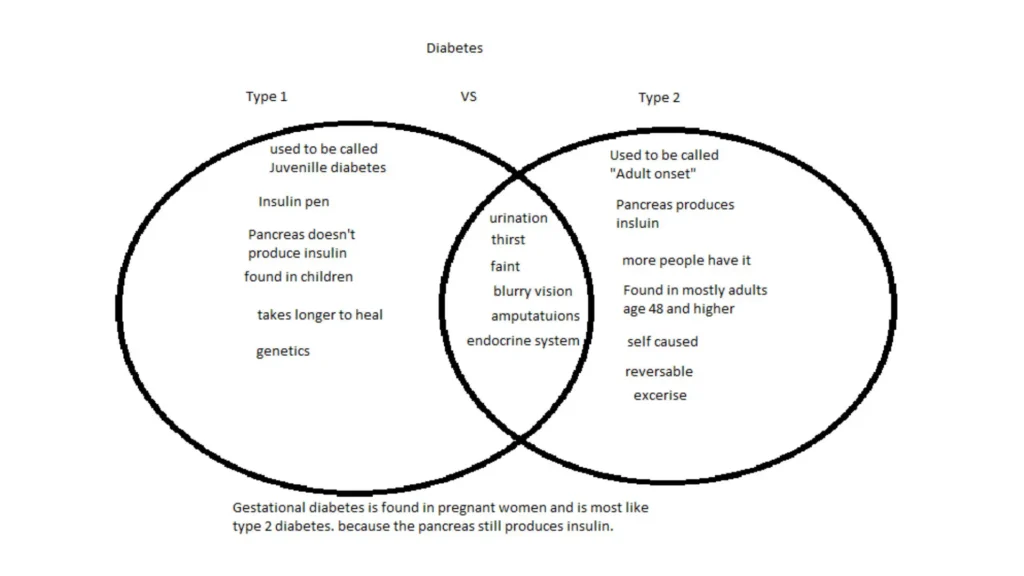
Type 2 Vs Type 1 Diabetes: Fundamental Differences
Type 2 vs type 1 diabetes are both part of diabetes mellitus but differ greatly. Type 1 diabetes is an autoimmune disease where the body attacks the insulin-making cells in the pancreas. This leads to a lack of insulin. Type 2 diabetes, on the other hand, is caused by insulin resistance and poor insulin production. It's often linked to lifestyle and genetics.
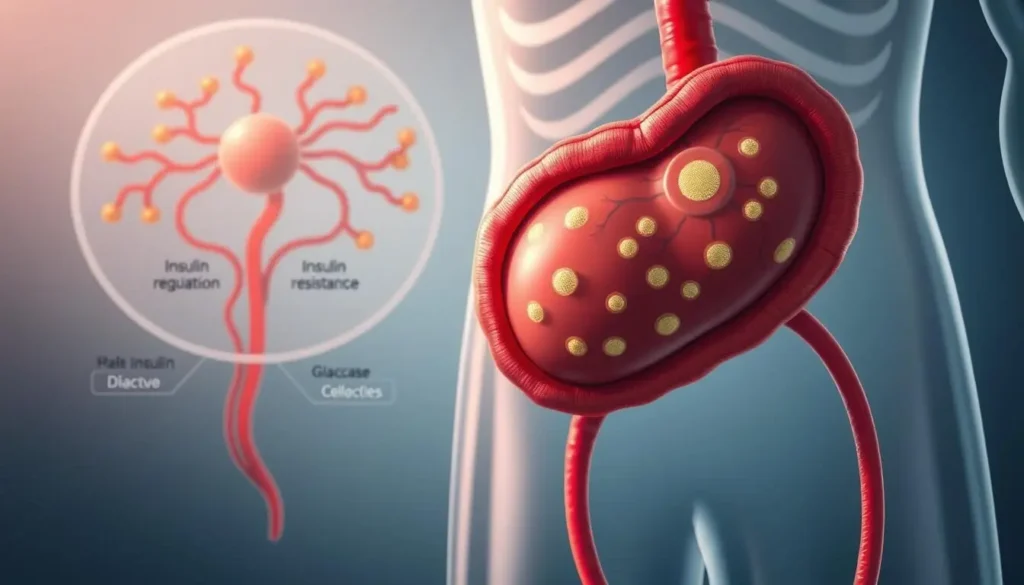
Pathophysiology Comparison
Type 1 diabetes is caused by the body's immune system destroying insulin-making cells in the pancreas. This results in a lack of insulin. Type 2 diabetes, by contrast, is due to insulin resistance. This means the body's cells don't use insulin well. Over time, the pancreas may also not make enough insulin.
Age of Onset Differences
Type 1 diabetes usually starts in children and young adults, but it can happen at any age. Type 2 diabetes, on the other hand, is more common in adults, often after 45. It's also seen in younger people due to rising obesity rates.
Genetic and Environmental Factors
Genetics play a big role in both types of diabetes. Type 1 diabetes has a strong genetic link due to autoimmune factors. Type 2 diabetes is influenced by both genetics and lifestyle factors. These include obesity, lack of exercise, and unhealthy eating.
| Characteristics | Type 1 Diabetes | Type 2 Diabetes |
|---|---|---|
| Primary Cause | Autoimmune destruction of beta cells | Insulin resistance and impaired insulin secretion |
| Typical Age of Onset | Children and young adults | Adults, specially after 45 |
| Genetic and Environmental Factors | Strong genetic predisposition, autoimmune | Genetic predisposition, obesity, inactivity, unhealthy diet |
Causes and Risk Factors
To fully understand diabetes, we must look at the causes and risk factors for type1 and type2 diabetes. Knowing these can help prevent and manage the disease.
Type1 Diabetes: Autoimmune Origins
Type1 diabetes happens when the body's immune system attacks the insulin-making cells in the pancreas. This leads to a lack of insulin, forcing those with type1 diabetes to take insulin.
Type2 Diabetes: Lifestyle and Hereditary Influences
Type2 diabetes is caused by a mix of genetics, lifestyle, and environment. A sedentary lifestyle, obesity, and bad diet are big risks. Family history also plays a part, making some more likely to get it.
Modifiable vs. Non-modifiable Risk Factors
Some risks, like age and genetics, can't be changed. But diet, exercise, and weight can be. Changing these can lower the chance of getting type2 diabetes.
Symptoms and Clinical Presentation
Knowing the symptoms of diabetes is key for early detection and treatment. Both type 2 vs type 1 diabetes have common signs that can greatly affect a person's life.
Common Symptoms in Both Types
Common signs of diabetes include feeling very thirsty and needing to urinate a lot. You might also feel tired and have blurry vision. These happen because your blood sugar is too high. It can make you dehydrated and blur your vision.
Unique Symptoms of Type 1 Diabetes
Type 1 diabetes often starts quickly and can lead to a serious condition called diabetic ketoacidosis. Symptoms can show up in a few weeks. People might lose a lot of weight and feel like they have the flu.
Gradual Onset in Type 2 Diabetes
Type 2 diabetes starts slowly, over years. Many people with type 2 diabetes don't notice symptoms until it's advanced. Regular health checks are important for catching it early.
It's important to know the differences in symptoms between type 2 vs type 1 diabetes. This helps doctors give the right treatment. Understanding these differences helps in creating better care plans.
Diagnosis and Testing Methods
Getting a correct diabetes diagnosis is key. Many tests are used to tell Type 2 vs Type 1 diabetes.
Blood Glucose Testing
Blood glucose testing is a main way to find out if you have diabetes. It checks your blood sugar levels, either at any time or after not eating for a while.
HbA1c Measurements
The HbA1c test shows your blood sugar levels over the last 2-3 months. It helps see how well you're managing your sugar.
Antibody Testing for Type 1
For Type 1 diabetes, antibody tests can confirm it's an autoimmune disease. They look for specific antibodies in your blood.
Differential Diagnosis Challenges
Telling Type 2 vs Type 1 diabetes can be hard because their symptoms are similar. Getting the right diagnosis is very important for the right treatment.
| Diagnostic Test | Type 1 Diabetes | Type 2 Diabetes |
|---|---|---|
| Blood Glucose Test | High levels, often with ketoacidosis | High levels, may not have ketoacidosis |
| HbA1c Measurement | Elevated, indicating poor glucose control | Elevated, indicating poor glucose control |
| Antibody Testing | Presence of specific autoantibodies | Typically negative for autoantibodies |
Treatment Approaches and Management
Diabetes treatment varies for type 1 and type 2. Each needs a different approach. Knowing these differences is key for good care.
Insulin Therapy Differences
Insulin therapy is vital for type 1 diabetes. The body can't make insulin. Type 2 diabetes might need insulin later, but first, other treatments are used.
Oral Medications for Type 2 Diabetes
Type 2 diabetes often uses oral meds to control blood sugar. These meds help in many ways, like making more insulin or making insulin work better.
| Medication Class | Mechanism of Action | Examples |
|---|---|---|
| Sulfonylureas | Stimulate insulin release | Glyburide, Glipizide |
| Metformin | Decreases hepatic glucose production | Glucophage |
| DPP-4 Inhibitors | Increase insulin release, decrease glucagon levels | Sitagliptin, Saxagliptin |
Lifestyle Modifications
Changing your lifestyle is key for both type 2 vs type 1 diabetes. This includes eating right and exercising.
Dietary Considerations
Eating a balanced diet is important. It should include fruits, veggies, whole grains, and lean proteins. Counting carbs can also help manage blood sugar.
Exercise Recommendations
Exercise is vital. It should include cardio and strength training. Aim for 150 minutes of moderate exercise a week.
Blood Glucose Monitoring
Checking blood sugar regularly is essential. It shows how diet, exercise, and meds affect your levels.
New and Emerging Treatments
New treatments for diabetes are being researched. This includes better insulin delivery, glucose monitoring, and new meds that could change the disease.
Prevention Strategies for Type 2 Diabetes
Preventing type 2 diabetes is possible. Stay healthy, exercise regularly, and eat well. These steps can delay or prevent the disease.
Conclusion: Living with Diabetes
Living with diabetes means you need to do many things to manage it well. You must check your blood sugar often, eat right, and follow your treatment plan. Knowing the difference between Type 2 vs Type 1 diabetes helps you meet your unique needs.
It's key to manage diabetes to avoid serious problems and keep a good quality of life. Good care includes medical treatment and making healthy lifestyle choices. Eating well and staying active are important. With the right care, people with diabetes can live full and happy lives.
Good diabetes care is a team effort. Healthcare providers, patients, and their families must work together. By sharing knowledge and support, people with diabetes can manage their condition better and feel better overall.