A prediabetes diagnosis can be a wake-up call, but it's far from a life sentence. In fact, it's an opportunity to take control of your health and steer yourself toward a healthier future.

With an estimated 98 million American adults living with prediabetes—and more than 80% of them unaware of it—understanding this condition is more critical than ever. This comprehensive guide will walk you through everything you need to know about prediabetes, from its subtle signs to actionable steps you can take to reverse it.
What is Prediabetes?
Prediabetes is a serious health condition where your blood sugar levels are higher than normal, but not yet high enough to be diagnosed as type 2 diabetes. Think of it as a warning sign. Your body isn't processing sugar (glucose) as efficiently as it should, which can lead to long-term damage to your heart, blood vessels, and kidneys if left unaddressed. The silver lining? Progression from prediabetes to type 2 diabetes isn't inevitable. With the right lifestyle changes, you can bring your blood sugar levels back to a healthy range.

The Silent Signals: Prediabetes Symptoms
One of the most challenging aspects of prediabetes is that it often presents with no clear symptoms. This is a primary reason why so many people are unaware they have it. However, in some cases, there might be subtle signs that can indicate you're at risk.
Some individuals with prediabetes may experience:
- Darkened skin: Patches of dark, velvety skin, a condition called acanthosis nigricans, may appear in the armpits, neck, or groin.
- Skin tags: These small skin growths often appear in the same areas as acanthosis nigricans.
- Increased thirst and frequent urination: As your blood sugar rises, your body tries to flush out the excess sugar through urine, leading to dehydration and increased thirst.
- Fatigue: Your cells may not be getting the glucose they need for energy, leaving you feeling tired and sluggish.
- Blurred vision: High blood sugar can affect the lenses in your eyes, causing temporary vision problems.
- Tingling or numbness: Some people with prediabetes may already have some nerve damage, causing tingling or numbness in their hands and feet.
It's important to remember that many people with prediabetes experience no symptoms at all. Therefore, understanding the risk factors is crucial for early detection.
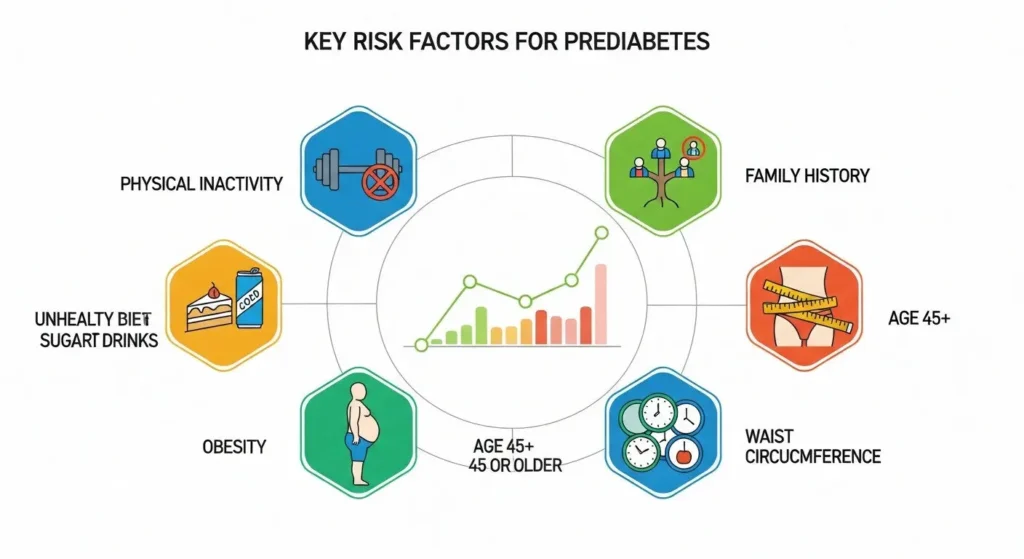
Are You at Risk? Key Factors for Prediabetes
Several factors can increase your likelihood of developing prediabetes. Some of these you can't change, like your genetics and age, while others are within your control.
Unmodifiable Risk Factors:
- Family History: Having a parent or sibling with type 2 diabetes significantly increases your risk.
- Age: The risk of prediabetes increases after the age of 35.
- Race and Ethnicity: Certain racial and ethnic groups, including African Americans, Hispanic Americans, Native Americans, and Asian Americans, have a higher risk.
- Gestational Diabetes: If you had diabetes during pregnancy, your risk of developing prediabetes later in life is higher.
Modifiable Risk Factors:
- Weight: Being higher weight or having obesity is a primary risk factor. Excess body fat, particularly around the abdomen, can lead to insulin resistance.
- Waist Size: A large waist circumference (over 40 inches for men and 35 inches for women) is a red flag for insulin resistance.
- Physical Inactivity: A sedentary lifestyle is a major contributor to prediabetes.
- Diet: A diet high in red and processed meats and sugar-sweetened beverages is associated with a higher risk.
- Smoking: Smoking can increase insulin resistance and the risk of type 2 diabetes.
- Sleep: Both a lack of quality sleep and conditions like obstructive sleep apnea can increase the risk of insulin resistance.
- High Blood Pressure and Cholesterol: Having high blood pressure or high levels of triglycerides (a type of fat in your blood) and low levels of “good” HDL cholesterol are associated with an increased risk.
- Polycystic Ovary Syndrome (PCOS): Women with PCOS have a higher risk of prediabetes.
Getting a Diagnosis: How to Know for Sure
Since prediabetes often has no symptoms, the only way to know for sure if you have it is through blood tests. Your doctor can order these tests as part of a routine check-up, especially if you have any of the risk factors mentioned above.
The most common tests for diagnosing prediabetes are:
- Fasting Plasma Glucose (FPG) Test: This test measures your blood sugar after you've fasted for at least eight hours.
- Normal: Below 100 mg/dL
- Prediabetes: 100 to 125 mg/dL
- Diabetes: 126 mg/dL or higher on two separate occasions
- A1C Test: This test provides your average blood sugar level over the past two to three months.
- Normal: Below 5.7%
- Prediabetes: 5.7% to 6.4%
- Diabetes: 6.5% or higher on two separate tests
- Oral Glucose Tolerance Test (OGTT): This test measures your blood sugar before and two hours after you drink a sugary liquid.
- Normal: Below 140 mg/dL after two hours
- Prediabetes: 140 to 199 mg/dL after two hours
- Diabetes: 200 mg/dL or higher after two hours
If your results fall within the prediabetes range, your doctor will likely recommend retesting at least once a year to monitor your blood sugar levels.
| Common Test | Normal | Prediabetes | Diabetes |
|---|---|---|---|
| Fasting Plasma Glucose (FPG) Test | < 100 mg/dl | 100 ~ 125 mg/dl | > 126 mg/dl |
| A1C Test | < 5.7% | 5.7% ~ 6.4% | > 6.5% |
| Oral Glucose Tolerance Test (OGTT) | < 140 mg/dl | 140 ~ 199 mg/dl | > 200 mg/dl |
The Power of Prevention: How to Reverse Prediabetes
The good news is that a prediabetes diagnosis is not a one-way street to type 2 diabetes. In fact, up to 50% of type 2 diabetes cases can be prevented or delayed with the right interventions. Lifestyle changes are the most powerful tool in your arsenal for reversing prediabetes.
1. Embrace a Healthy Diet
What you eat plays a significant role in managing your blood sugar levels. There's no single “prediabetes diet,” but the focus should be on whole, unprocessed foods.
- Fill Your Plate with Non-Starchy Vegetables: Aim to have half of your plate filled with vegetables like leafy greens, broccoli, and peppers.
- Choose Lean Protein: Include lean protein sources like chicken, turkey, fish, tofu, and legumes.
- Opt for Healthy Carbohydrates: Choose whole grains like brown rice, quinoa, and whole-wheat bread over refined carbohydrates.
- Incorporate Healthy Fats: Healthy fats found in avocados, nuts, and olive oil can be beneficial.
- Limit Added Sugars and Processed Foods: Reduce your intake of sugary drinks, desserts, and processed snacks.
- Stay Hydrated: Drink plenty of water throughout the day.
For personalized dietary advice, consider consulting a registered dietitian who can help you create a sustainable eating plan.

2. Get Moving: The Importance of Physical Activity
Regular exercise is crucial for improving insulin sensitivity and lowering blood sugar levels. Aim for at least 150 minutes of moderate-intensity aerobic exercise per week, which breaks down to about 30 minutes a day, five days a week.
Examples of moderate-intensity exercise include:
- Brisk walking
- Cycling
- Swimming
- Dancing
- Water aerobics
In addition to aerobic activity, incorporate strength training exercises at least two to three times a week. Building muscle helps your body use glucose more effectively. Remember to consult your doctor before starting any new exercise program.

3. Manage Your Weight
If you're higher-weight person, losing even a small amount of weight can make a significant difference. Losing just 5% to 7% of your body weight can reduce your risk of developing type 2 diabetes by 58%.
4. Quit Smoking
Smoking damages cells in your body and can make it harder for your body to use insulin effectively. Quitting smoking is one of the best things you can do for your overall health and to reduce your risk of diabetes.
5. Prioritize Quality Sleep
Aim for 7-9 hours of quality sleep per night. If you have a sleep disorder like sleep apnea, getting it treated is essential for improving your insulin sensitivity.
The Long-Term Picture: Complications of Untreated Prediabetes
Ignoring prediabetes can have serious consequences. The long-term damage associated with diabetes, particularly to your heart, blood vessels, and kidneys, may already be starting during the prediabetic stage. Untreated prediabetes can progress to type 2 diabetes, which increases your risk of:
- Heart disease and stroke
- Kidney disease
- Nerve damage (neuropathy)
- Eye damage and vision loss (retinopathy)
- Foot complications that can lead to amputation
Prediabetes in Children and Adolescents
Prediabetes is not just a condition that affects adults. The prevalence of prediabetes in children and adolescents is on the rise, largely due to the increase in childhood obesity. The risk factors and diagnostic criteria are generally the same for children as for adults. If you're concerned about your child's risk, talk to their pediatrician about screening.
Take the First Step Today
A prediabetes diagnosis is a call to action, not a reason to panic. By making sustainable lifestyle changes, you have the power to reverse this condition and significantly reduce your risk of developing type 2 diabetes. Talk to your doctor, get tested if you're at risk, and take the first step toward a healthier you today.