Diabetes is a chronic health condition affecting how your body turns food into energy. When you have diabetes, your body either doesn't make enough insulin or can't use it effectively, causing high blood sugar levels that can lead to serious health problems. With proper understanding and management, people with diabetes can lead healthy, active lives. This comprehensive guide explores the types of diabetes, symptoms, risk factors, and modern approaches to managing this common condition.

What Is Diabetes?
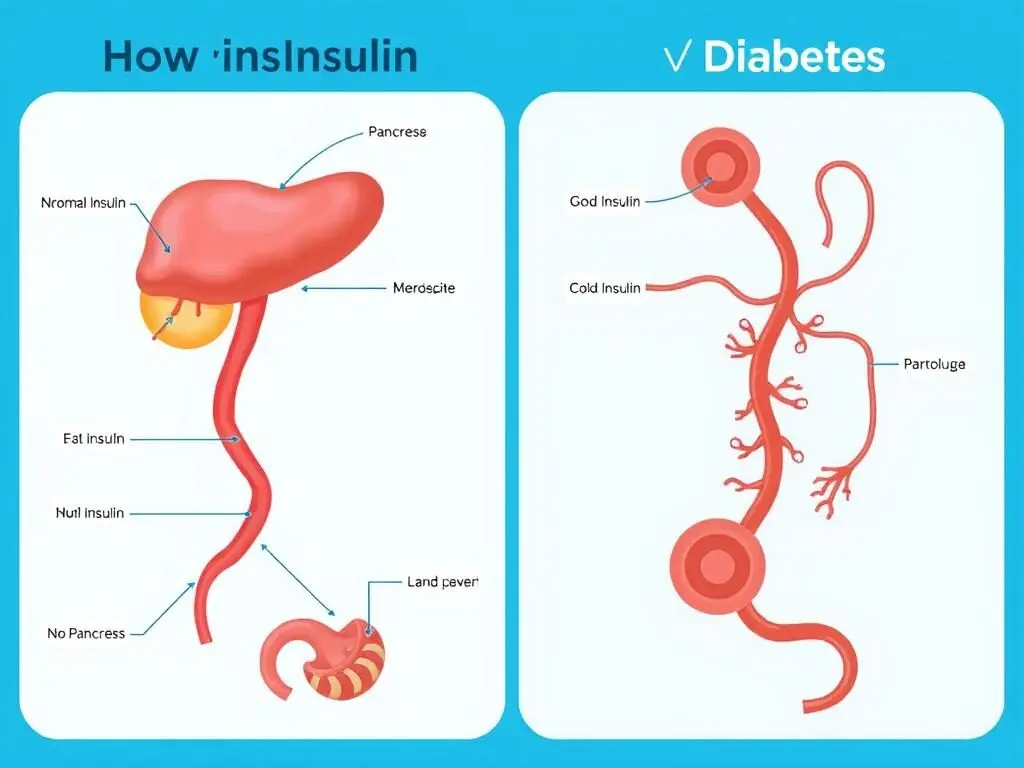
Diabetes mellitus, commonly known as diabetes, is a disease that occurs when your blood glucose (blood sugar) is too high. Blood glucose is your body's main source of energy and comes from the food you eat. Insulin, a hormone made by the pancreas, helps glucose enter your cells to be used for energy. If your body doesn't make enough insulin, or if your cells don't respond properly to insulin, glucose stays in your bloodstream and doesn't reach your cells.
Over time, having too much glucose in your blood can cause health problems. Although diabetes has no cure, you can take steps to manage your diabetes and stay healthy.
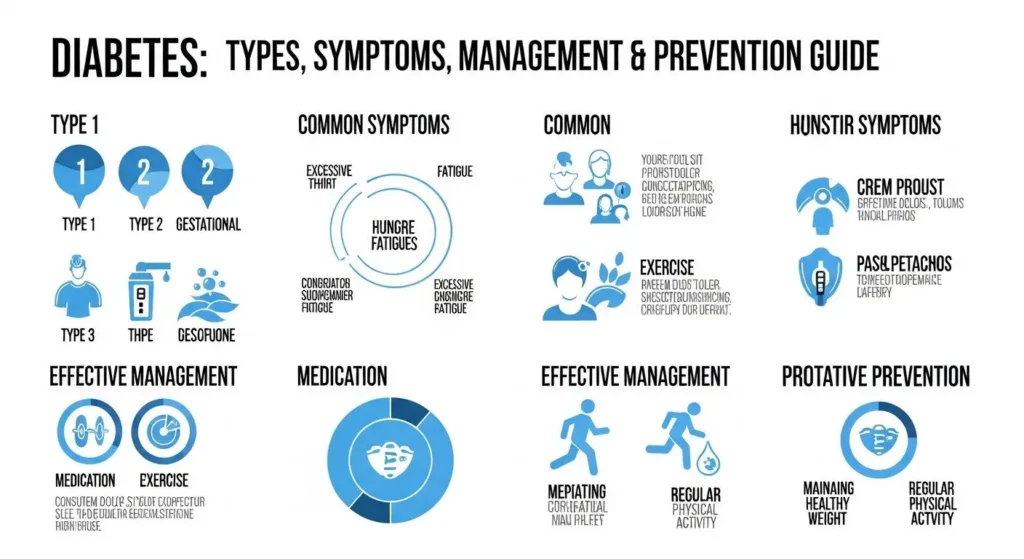
Types of Diabetes
There are several types of diabetes, each with different causes and risk factors:
Type 1 Diabetes
Type 1 diabetes is an autoimmune disease where the immune system attacks and destroys insulin-producing cells in the pancreas. As a result, your body produces little or no insulin. Type 1 diabetes accounts for about 5-10% of all diabetes cases and is usually diagnosed in children, teenagers, and young adults, though it can develop at any age.

Type 2 Diabetes
Type 2 diabetes is the most common form, accounting for 90-95% of diabetes cases. With type 2 diabetes, your body doesn't use insulin properly (insulin resistance) and can't make enough insulin to overcome this resistance. While it mainly affects adults, increasing rates of obesity have led to more children developing this condition. Many people with type 2 diabetes don't know they have it.

Gestational Diabetes
Gestational diabetes develops during pregnancy in women who don't already have diabetes. It usually goes away after giving birth, but it increases the risk of developing type 2 diabetes later in life. The condition affects the way cells use glucose and can cause high blood sugar that may affect the pregnancy and the baby's health.

Other Types of Diabetes
Less common types include monogenic diabetes (such as maturity-onset diabetes of the young or MODY), which results from genetic mutations, and type 3c diabetes, which occurs due to pancreatic damage from conditions like pancreatitis or pancreatic cancer.
Approximately 37.3 million people in the United States have diabetes, which is about 11% of the population. Type 2 diabetes is the most common form, representing 90% to 95% of all diabetes cases.
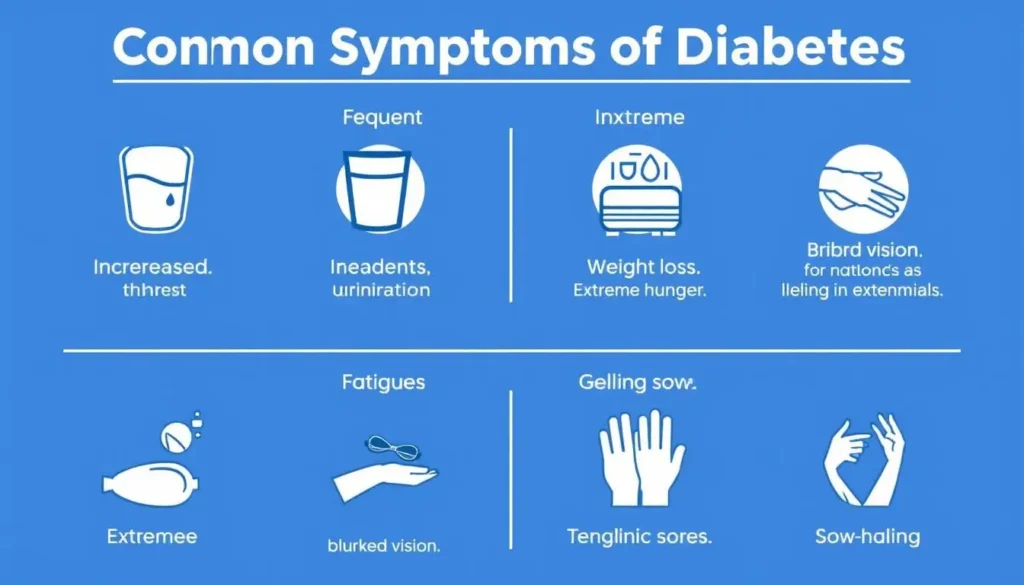
Symptoms and Signs of Diabetes
The symptoms of diabetes can vary depending on how high your blood sugar is elevated. Some people, especially those with prediabetes or type 2 diabetes, may not experience symptoms initially. However, as the disease progresses, common symptoms include:
Common Diabetes Symptoms
- Increased thirst (polydipsia)
- Frequent urination
- Extreme hunger
- Unexplained weight loss
- Fatigue
- Blurred vision
- Slow-healing sores
- Frequent infections
- Numbness or tingling in hands/feet
Symptoms by Diabetes Type
Type 1 diabetes: Symptoms often develop quickly over weeks or months and can be severe. Additional symptoms may include nausea, vomiting, and stomach pains.
Type 2 diabetes: Symptoms develop slowly, sometimes over several years, and may be so mild that you don't notice them.
Gestational diabetes: Often has no noticeable symptoms. It's usually detected through routine screening tests during pregnancy.
Warning: If you experience symptoms of severe high blood sugar such as very dry mouth, extreme thirst, hot and dry skin, confusion, or loss of consciousness, seek immediate medical attention. These could be signs of diabetes-related ketoacidosis (DKA) or hyperosmolar hyperglycemic state (HHS), which are life-threatening emergencies.
Risk Factors for Diabetes
Understanding the risk factors for diabetes can help with early detection and prevention. Risk factors vary by diabetes type:
Type 1 Diabetes Risk Factors
- Family history (parent or sibling with type 1)
- Certain genetic factors
- Age (can occur at any age but often appears during childhood or adolescence)
- Environmental factors (though not well understood)
Type 2 Diabetes Risk Factors
- Being higher weight or having obesity
- Age 35 or older
- Family history of diabetes
- Physical inactivity
- History of gestational diabetes
- Prediabetes
- Race/ethnicity (higher risk in African American, Hispanic/Latino, Native American, and Asian American populations)
- High blood pressure
- Polycystic ovary syndrome (PCOS)
Gestational Diabetes Risk Factors
- Higher weight or obesity
- Family history of diabetes
- Previous gestational diabetes
- Having given birth to a baby weighing over 9 pounds
- Polycystic ovary syndrome
- Age (over 25)
- Certain racial/ethnic backgrounds
Long-Term Complications of Diabetes
Consistently high blood glucose levels can lead to serious complications over time. Managing your diabetes effectively helps reduce the risk of developing these complications:
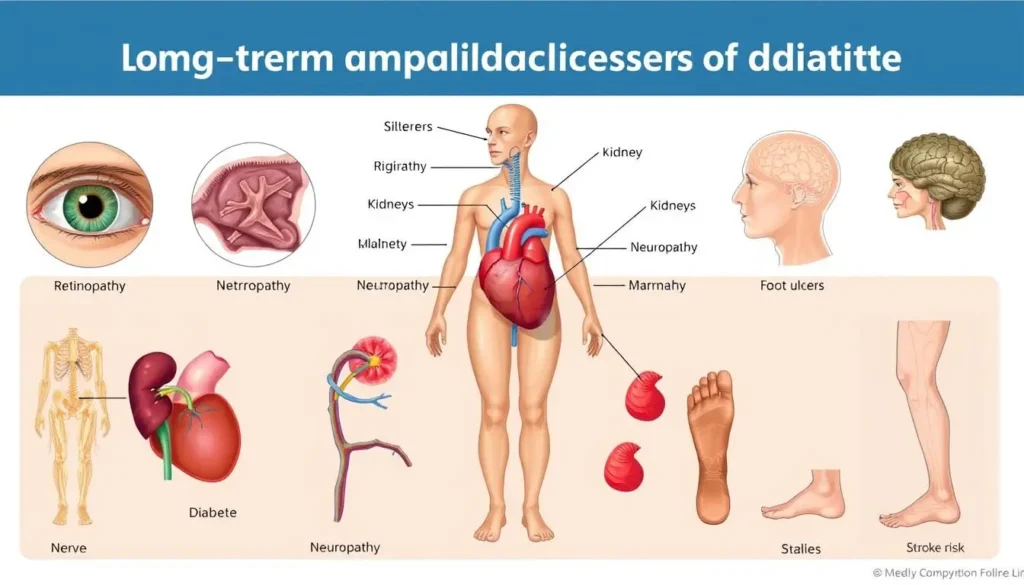
Cardiovascular Complications
Diabetes significantly increases the risk of various cardiovascular problems, including:
- Coronary artery disease
- Heart attack
- Stroke
- Atherosclerosis (narrowing of arteries)
- High blood pressure
Nerve Damage (Neuropathy)
Excess sugar can injure the walls of tiny blood vessels that nourish your nerves, especially in the legs. This can cause tingling, numbness, burning or pain that usually begins at the tips of the toes or fingers and gradually spreads upward.
Kidney Damage (Nephropathy)
Diabetes can damage the blood vessels in your kidneys, affecting their ability to filter waste from your blood. Severe damage can lead to kidney failure or irreversible end-stage kidney disease, requiring dialysis or a kidney transplant.
Eye Damage (Retinopathy)
Diabetes can damage blood vessels in the retina, potentially leading to blindness. It also increases the risk of other serious vision conditions, such as cataracts and glaucoma.
Foot Damage
Nerve damage in the feet or poor blood flow can increase the risk of various foot complications. Left untreated, cuts and blisters can develop serious infections that may ultimately require toe, foot or leg amputation.
People with diabetes are 2-3 times more likely to have depression than people without diabetes. Mental health is an important aspect of diabetes management.
Diagnosing Diabetes
Healthcare providers use several blood tests to diagnose diabetes and prediabetes:
| Test Type | Normal Range | Prediabetes | Diabetes |
| Fasting Blood Glucose Test | Less than 100 mg/dL | 100-125 mg/dL | 126 mg/dL or higher |
| A1C Test | Below 5.7% | 5.7% to 6.4% | 6.5% or higher |
| Random Blood Glucose Test | N/A | N/A | 200 mg/dL or higher with symptoms |
| Oral Glucose Tolerance Test | Less than 140 mg/dL | 140-199 mg/dL | 200 mg/dL or higher |
For gestational diabetes, healthcare providers typically perform screening between 24 and 28 weeks of pregnancy using the glucose challenge test and, if needed, an oral glucose tolerance test.

Managing Diabetes
Diabetes management involves several key strategies working together to keep blood glucose levels within a healthy range. A comprehensive approach includes:
Blood Sugar Monitoring
Regular monitoring of blood glucose levels is essential for diabetes management. Depending on your treatment plan, you may need to check your blood sugar levels several times a day or use a continuous glucose monitor (CGM) that tracks levels throughout the day and night.

Medications and Insulin
Depending on the type of diabetes you have, medication may be necessary:
- Type 1 diabetes: Requires insulin therapy for life, delivered via injections or an insulin pump.
- Type 2 diabetes: May be managed with lifestyle changes alone or may require oral medications, injectable medications, or insulin.
- Gestational diabetes: Often managed with diet and exercise, but some women may need insulin.

Healthy Eating
A balanced diet is crucial for managing diabetes. Focus on:
- Consistent carbohydrate intake
- Portion control
- Regular meal timing
- Emphasis on fruits, vegetables, whole grains, and lean proteins
- Limiting refined carbohydrates and added sugars
- Monitoring fat intake, especially saturated fats

Regular Physical Activity
Exercise helps lower blood glucose levels and improves insulin sensitivity. Aim for:
- At least 150 minutes of moderate-intensity aerobic activity weekly
- Strength training exercises at least twice a week
- Breaking up long periods of sitting with short activity breaks

Preventing Type 2 Diabetes
While type 1 diabetes cannot currently be prevented, you can take steps to reduce your risk of developing type 2 diabetes and gestational diabetes:
Effective Prevention Strategies
- Maintain a healthy weight or lose weight if higher weight
- Be physically active for at least 30 minutes, 5 days a week
- Eat a balanced diet rich in fruits, vegetables, and whole grains
- Limit processed foods and added sugars
- Quit smoking
- Manage stress effectively
- Get adequate sleep (7-9 hours nightly)
- Limit alcohol consumption
Risk Factors You Cannot Change
- Family history of diabetes
- Age (risk increases after 35)
- Race/ethnicity
- History of gestational diabetes
- Polycystic ovary syndrome
- Certain genetic predispositions

If you have prediabetes, losing just 5-7% of your body weight through diet and exercise can reduce your risk of developing type 2 diabetes by up to 58%.
Living With Diabetes
Living with diabetes requires daily attention to your health, but it shouldn't prevent you from enjoying a full and active life. Here are some strategies for successfully managing diabetes long-term:
Building Your Diabetes Care Team
A comprehensive diabetes management plan typically involves several healthcare professionals:
- Primary care physician
- Endocrinologist (diabetes specialist)
- Certified diabetes care and education specialist
- Registered dietitian
- Eye doctor
- Podiatrist (foot doctor)
- Dentist
- Mental health professional
Regular Health Checkups
Regular monitoring helps prevent complications. Schedule:
- A1C tests 2-4 times per year
- Annual eye exams
- Regular foot exams
- Dental checkups twice yearly
- Annual kidney function tests
- Regular blood pressure and cholesterol checks
Mental Health and Emotional Well-being
Living with a chronic condition like diabetes can be emotionally challenging. Pay attention to your mental health by:
- Joining diabetes support groups
- Practicing stress management techniques
- Seeking professional help if you experience depression or anxiety
- Being open with friends and family about your needs

Special Considerations
Managing diabetes requires additional planning in certain situations:
- Travel: Pack extra supplies, carry medications in original packaging, and plan for time zone changes.
- Illness: Continue taking medications, check blood sugar more frequently, and stay hydrated when sick.
- Exercise: Monitor blood sugar before, during, and after physical activity, and adjust food or medication as needed.
- Extreme weather: Protect insulin and testing supplies from temperature extremes.

Taking Control of Your Diabetes
Diabetes is a complex condition that requires ongoing attention, but with proper management, you can lead a healthy, active life. Understanding your condition, working closely with healthcare providers, making healthy lifestyle choices, and staying informed about the latest diabetes care advances are all essential parts of successful diabetes management.
Remember that diabetes management is highly individualized. What works for one person may not work for another. Be patient with yourself as you learn to manage your condition, and don't hesitate to ask for help when needed.
How often should I check my blood sugar if I have diabetes?
The frequency of blood sugar monitoring varies based on your type of diabetes, treatment plan, and overall health. People with type 1 diabetes typically check 4-10 times daily, while those with type 2 diabetes might check less frequently. Your healthcare provider will recommend a monitoring schedule that's right for you.
Can diabetes be cured?
Currently, there is no cure for diabetes. Type 1 diabetes requires lifelong insulin therapy. Some people with type 2 diabetes can achieve remission through significant weight loss, either from bariatric surgery or intensive lifestyle changes, but the underlying genetic predisposition remains. Ongoing monitoring and healthy habits are still necessary even in remission.
What should I do if my blood sugar is too high or too low?
For high blood sugar (hyperglycemia), follow your doctor's instructions, which may include taking additional insulin or medication. Stay hydrated and monitor your levels closely. For low blood sugar (hypoglycemia), follow the 15-15 rule: consume 15 grams of fast-acting carbohydrates (like glucose tablets or juice), wait 15 minutes, and recheck your blood sugar. Repeat if necessary. Severe cases of either condition require immediate medical attention.